
Back Pain
BACK PAIN
Causes
Mechanical problems: Arise due to disc degeneration i.e. breaking down of shock absorber with age. This leads to pain when the back is stressed. Other cause includes, wearing down of the facet joints, spasm of muscle and disc herniation.
Spine Injuries: Such as sprains (tears in supporting ligaments) and fractures leading to acute or chronic back pain. Fractures are the result of fall or accidents and also due to osteoporosis, which causes weak and porous bones.
Acquired conditions: Spondylolisthesis i.e. slippage of one vertebrae over other leading to nerve compression. Various types of arthritis, like osteoarthritis, rheumatoid arthritis and ankylosing spondylitis. Spinal Canal Stenosis i.e. narrowing of the spinal canal, which puts pressure on the nerves.
Infections: Such as Tuberculosis are very common in India. They may lead to chronic pain even when treated for prolonged time with medication due to structural change in the spine. Other bacterial infection can be cause of acute severe pain which requires early diagnosis and management.
Tumors: Though rare but can be a cause of severe debilitation as in case of metastatic disease and require palliative pain treatment, to improve quality of life in these individuals.
Others: Include pregnancy, fibromyalgia, kidney stones or infections and endometriosis. Untreated depression and anxiety can make back pain feel much worse. Insomnia, or the lack of sleep, can also contribute to back pain.
What is a Facet and Sacroiliac Joint (SI) Rhizotomy?
Facet and sacroiliac joint conditions can be very painful. If the pain does not subside with chiropractic care, physical therapy, medication and other non-invasive treatments, injections may be considered. Rhizotomy involves placing a RF cautery probe into the joint. When the tip of the probe is heated, it cauterizes tiny nerve fibers in the joint.
Depending on the response to these injections, rhizotomy may be considered. Results of the procedure may not be permanent, but generally last much longer than injections. Rhizotomy is the same as a denervation or neurotomy procedure.
Rhizotomy is used to treat painful facet joints and sacroiliac joints.
What is Minimally Invasive Spinal Surgery?
Minimally invasive spinal surgery does not apply to any one particular type of surgery. The goal of this type of spinal surgery is to achieve the same effect as with traditional surgery, but to do so through small incisions.
This also involves less trauma to muscles. Surgery is sometimes done through small tubes. There are minimally invasive techniques for several spinal surgeries, including Discectomy and fusion. However, this method cannot be applied to all patients. Often, a minimally invasive method of placing pedicle screws and rods is combined with a traditional fusion.
Minimally invasive surgery techniques include a variety of different surgery types and are sometimes used in conjunction with other spinal surgery procedures to treat Spondylolisthesis, herniated disc, degenerated disc and possibly other conditions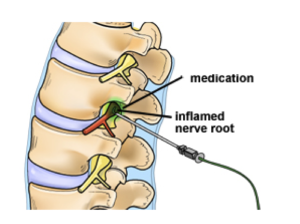
Dr Abhinav Gupta is the best pain specialist in Delhi with over 5000 procedures to his credit in last 18 years. Dr Abhinav has done his MBBS from Armed forces Medical College (AFMC) then did his Surgical Neurology training at Sir Gangaram Hospital (SGRH) for 6 years. Dr Abhinav Gupta has been trained at Best Pain Centers in the world. He has done fellowship in Minimally Invasive Spine Surgery from UNIVERSITY OF CHICAGO, USA and PAIN FELLOWSHIP from Asceulap Academy, Switzerland. He has been trained in palliative treatment for Cancer Pain.
The Best pain specialist in Delhi gives protocol based treatment for all type of Painful conditions .The Best Pain management protocols are followed at our centers.
Best Pain Treatment in Delhi, NCR
Protocol at Neuro Spine and Pain Clinic (NSP Clinic)
Dr Abhinav Gupta and his team follow a step ladder approach
The cause of the pain is ascertained by meticulous History and Examination protocol developed by Dr Abhinav Gupta
Following investigations are adviced depending on the patient’s condition
Blood tests, X-rays, CT scans, MRI, Pain Intensity Scoring-ALGOMETRY, Psychology Assessment, Endoscopy, Arthritis Protocol and PET or SPECT
Intensive battery of test is followed by
Customised Pain Treatment
The pain treatment is designed specifically for the patient and is followed according to International standards once the patient gives consent for starting the treatment.
The treatment may consist of oral medication, physical therapy, psychotherapy, Injections, Percutaneous interventions; Ozone, PRP therapy, Endoscopy or surgery.
- Radiofrequency Ablation/Lesioning 30 K
- Pain Free Epidural Injections 10 k
- Vertebroplasty 50 K
- Balloon Kyphoplasty 100 K
- Percutaneous Endoscopic Discectomy 100 K-125K for 2
- Ozone procedures(3 sitting) 25K
- RF Trigeminal Lesioning 30 K
- Cervical /lumbar/SI /facet blocks 5k /site or level
- Spinal Epiduroscopy ( adhesiolysis) 75 K
- Endoscopic Spinal fusion 100 K plus implant
- Spinal Cord Stimulation 100k plus implant
- Botox injections EMG guided 10K + own injection
- PRP therapy 30 K
- LASERS 20 K to 50 K
- Varicose veins LASERS 100K
- counseling session 2k 1 day intense with music therapy
Pain procedures for them have been explained in detail for the patients.
Pain Free Epidural Injections: These injections consisting of local anesthetics /analgesics in combination with, given via small openings from where the nerve roots exit. These injections reduce the swelling caused by inflammation to the area thus reducing pain and numbness.
These injections are given at various sites like cervical, dorsal and lumbar.
Indications
Spinal Cord Stimulation (SCS): It is a procedure done for relieving pain of neuropathic origin. Electrodes are implanted surgically in the spinal canal, which delivers low electrical signals to the spinal cord /nerves thus blocking the pain signals. SCS is implanted when other nonsurgical treatments have failed and surgery is unlikely to help.
Indications -Failed Back Surgery syndrome (FBSS) pain, Complex Regional Pain Syndrome (CRPS), Complex Peripheral Neuropathy, Phantom limb pain and Angina/Ischemic limb pain..
Radiofrequency Ablation (RFA): It is a procedure which is used to reduce chronic (long lasting) pain. The radio waves are used to at particular frequency to produce heat in particular area of the nerve which is causing the pain. The pain fibers are modulated and pain is relived till the new fibers are regenerated. This is associated with minimal to no side effects and generally well tolerated.
Indications – low backache, Trigeminal Neuralgia.
Ozone Discectomy (Ozone-nucleolysis): Injection of Ozone-Oxygen mixture into the disc for treating patients with back and leg pain (sciatica).
Among working-age people, as many as 20 percent experience back symptoms at least every year. Facet arthropathy, sciatica, muscle strain, sacroilitis, bulging or herniated discs and degenerative disc disease. Prolapsed Intervertebral Discs (PIVD) are the most common cause of low back pain associated with a defined structural Abnormality.
.
Different Non Surgical Interventions Employed Successfully:
- Epidural Steroid Inj.
- Epidurogram & Epidurolysis.
- Nerve root sleeve/ Transforaminal Inj.
- Intra-discal steroid inj.
- Nucleoplasty- Thermal & Mechanical
- Ozone Discolysis
Conventional treatment methods for back pain comprise laminectomy/ Discectomy microsurgery, endoscopic Discectomy and Percutaneous Discectomy, among others. These are invasive methods and their goal is to remove or contain the protruding disc. However, these methods have occasionally demonstrated a discrete incidence of failure and/or recurrence. Outcome studies of lumber disc surgeries ranging from 4% to 15%, have been noted. “In case of surgery, the chance of recurrence of pain is nearly 15 percent as against less than three percent in Ozone treatment. The reason for failure in conventional surgeries are: Dural fibrosis, Arachnoidal adhesions, Muscles and fascial fibrosis. The mechanical instability resulting from the partial removal of bony & ligamentous structures required for surgical exposure & decompression and presence of Neuropathy are some of the etiologies left unaddressed surgically.
Understanding the need for Nano -Technology
- The various treatment options have confused clinicians and investigators due to high failure rate and complications associated with different kinds of surgeries and interventions. There has been a surge of interest in the search for a safer alternative method of decompressing the nerve roots maintaining the structural stability.
- Another safe least invasive alternative therapy that has been receiving exposure in Europe is the use of medical Ozone (02/03 mixture) in the treatment of PIVD. Epidural steroid injection, Transforaminal epidural decompressions has a high success rate (up to 85%), but chances of recurrences are there specially if these interventions are done at later stage. anaphylaxis following intradiscal chymopapain injection. Injection of Ozone for discogenic radiculopathy (low back pain with radiation to legs) has developed as a revolutionary alternative to chemonucleolysis and disc surgery .
The use of ozone revolution for treating disc diseases
Muto suggested an intradiscal injection of Ozone for a disc Ozone injection into the intervertebral disc. It is very important to note from those reports that complications are remarkably few. Not a serious single life-threatening complication was found even after 120,000 cases of Ozone nucleolysis, which stresses the safety of these procedures.
The most critical portion of performing any of the minimally invasive procedures is the accuracy and safe positioning of the needle (or terminal device) in the centre of the disc space. The risk in ozonucleolysis is particularly minimised, with the use of a very thin 22/25-gauge needle. It may take anywhere from 5 to 30 minutes to position a needle in the centre of the disc space under radiological guidance. Once the needle is safely placed in position, ozonucleolysis is completed in only another 2 to 3 minutes.
How is water contained within the domain of proteoglycans?
The water binding capacity of the proteoglycan molecule is partially a property of its size and physical shape, but the main force that holds water to the molecule stems from the ionic, carboxyl (COOH) and sulphate (SO4) radicals of the glycosaminoglycan chains. The ozone can have a direct effect on these carboxyl and sulphate groups, breaking down some of these glycosaminoglycan chains which make up the proteoglycans. The destruction of these cross-linked structures reduces their ability to hold water therefore diminishing the size of the herniation by collagen fibers and signs of regression (vacuole formation and fragmentation)- a sort of disk strong mummification
By inhibiting inflammatory Nociceptors, Synthesis of Prostaglandins & Secretion of Proteinases, Liberation of Bradykinin and Pain Inducing Products. Several studies suggest disc inflammation as a mechanism of sciatica due to disc herniation. Ozone has been shown to have an effect on the inflammatory cascade by inhibiting synthesis of pro-inflammatory prostaglandins or release of bradykinin or release of algogenic compounds; increased release of antagonists or soluble receptors able to neutralize pro-inflammatory cytokines like interleukin (IL)-1, IL-2, IL-8, IL-12, IL-15 and interferon, and tumor necrosis factor. Therefore, by reducing the inflammatory components there is a corresponding reduction in pain.
By stimulating fibroblasts & immunosuppressor cytokines
- Local production of Antioxidant Enzymes
- Another action which may prove to be one of the most important is the stimulation and Release of immune-suppressor cytokines like transforming growth factor, and IL-10 fibroblastic activity by ozone. Fibroblasts initiate the repair process by stimulating the deposition of collagen. Although yet to be validated, this mode of action could explain the resolution of PIVD on CT scans and the small percentage of patients who have relapses after the completion of treatment plan.
- Ozone may have a reflex therapy effect called ‘chemical acupuncture’, breaking the chain of infectionwhich is healed with antibiotics.
In fact, over 120,000 patients have been treated successfully worldwide using the injection of medical ozone with a success rate of 80-90% and with a near nil rate of procedure-related complications. “The procedure is a safe and effective alternative to open surgical procedure. Patients get the advantage of going home after a short recovery on the same day. They generally go to work within a week and is spared prolonged absence from work and disability,” The treatment relieves pain substantially and, after two sittings, people “can go back to work under medical guidance”.
Comparison: 1. More hospital stay One day/day care 2. Complications of prolonged surgery& spine surgery is the treatment of choice for prolapsed disc (PIVD) done under local anaesthesia in a daycare setting. This procedure is ideally suited for cervical & lumbar disc herniation with radiculopathy. The total cost of the procedure is much less than that of surgical discectomy. All these facts have made this procedure very popular in European countries. It is also gaining popularity in our country due to high success rate, less invasiveness, fewer chances of recurrences, remarkably fewer side effects meaning high safety profile, short hospital stay, no post-operative discomfort or morbidity and low cost.
Surgery: Having back surgery can be a difficult choice. Typically, people consider surgery for back pain only after all other treatments have failed to provide relief. Even then, surgery does not provide significant improvement for everyone. And while the risks of back surgery are generally low, they can be serious in some people.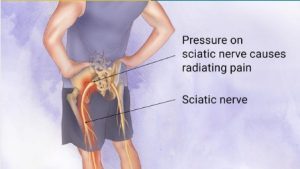
What is sciatic pain or sciatica?
Sciatic pain or sciatica is the pain that occurs because a nerve coming from the spinal cord is pressed on (trapped) by a prolapsed disc, or is irritated by the inflammation caused by the prolapsed disc. Although the problem is in the back, you feel pain along the course of the nerve in addition to back pain. Therefore, you may feel pain down a leg to the calf or foot. Sciatic pain can range from mild to severe, but it is often worse than the back pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. The sciatic nerve is a large nerve that is made up from several smaller nerves that come out from the spinal cord in the lower back. It travels deep inside the buttock and down the back of the leg. There is a sciatic nerve for each leg.
Treatment of back pain and sciatic pain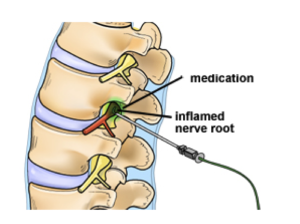
What is sciatic pain or sciatica?
Sciatic pain or sciatica is the pain that occurs because a nerve coming from the spinal cord is pressed on (trapped) by a prolapsed disc, or is irritated by the inflammation caused by the prolapsed disc. Although the problem is in the back, you feel pain along the course of the nerve in addition to back pain. Therefore, you may feel pain down a leg to the calf or foot. Sciatic pain can range from mild to severe, but it is often worse than the back pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. The sciatic nerve is a large nerve that is made up from several smaller nerves that come out from the spinal cord in the lower back. It travels deep inside the buttock and down the back of the leg. There is a sciatic nerve for each leg.
Treatment of sciatic pain
Spinal Injections: Injections like the Cervical, Thoracic and Lumbar Interlaminar Epidural Injections and Transforaminal injection are injections into the opening at the side of the spine where a nerve roots exits. These injections reduce the inflammation and swelling of spinal nerve roots and other tissues surrounding the spinal nerve root and reduces pain, tingling and numbness and other symptoms caused by such inflammation, irritation or swelling.
Spinal cord stimulation: Spinal cord stimulation is a procedure that delivers low-level electrical signals to the spinal cord or to specific nerves to block pain signals from reaching the brain. Spinal cord stimulation is recommended when other treatments have not been successful, when surgery is not likely to help, or when surgery has failed.
Radiofrequency Ablation: Radiofrequency ablation (or RFA) is a procedure used to reduce pain. An electrical current produced by a radio wave is used to heat up a small area of nerve tissue, thereby decreasing pain signals from that specific area. RFA can be used to help patients with chronic (long-lasting) low-back pain. RFA has proven to be a safe and effective way to treat some forms of pain. It also is generally well-tolerated, with very few associated complications.
Ozone Discectomy (Ozonucleolysis): Injection of Ozone-Oxygen mixture into the disc is a new alternative method of treating patients suffering from back and leg pain (sciatica) caused by disc prolapse. Large number of international studies confirms the efficacy of this treatment and superiority of this treatment over conventional disc surgery.
Surgery: Having back surgery can be a difficult choice. Typically, people consider surgery for back pain only after all other treatments have failed to provide relief. Even then, surgery does not provide significant improvement for everyone. And while the risks of back surgery are generally low, they can be serious in some people.
At NSP clinic , we provide the best and latest non- surgical interventions to treat sciatic pain and sciatica
What is slipped disc?
When you have a prolapsed disc (commonly called a slipped disc), a disc does not actually slip. What happens is that part of the inner softer part of the disc (the nucleus pulposus) bulges out (herniates) through a weakness in the outer part of the disc. A prolapsed disc is sometimes called a herniated disc. The bulging disc may press on nearby structures such as a nerve coming from the spinal cord. Some inflammation also develops around the prolapsed part of the disc.
Any disc in the spine can prolapse. However, most prolapsed discs occur in the lumbar part of the spine (lower back). The size of the prolapse can vary. As a rule, the larger the prolapse, the more severe the symptoms are likely to be.
Who gets a slipped disc?
Bouts of back pain are very common. However, less than 1 in 20 cases of acute (sudden onset) back pain are due to a prolapsed disc. (Most cases of back pain are classed as simple low back pain. This is thought to be caused by a minor problem in a muscle, ligament, or other structure in the back – for example, a strained muscle.) The most common age to develop a prolapsed disc is between 30 and 50 years. Twice as many men as women are affected.
How is it caused?
It is not clear why some people develop a prolapsed disc and not others, even when they do the same job or lift the same sort of objects. It seems that some people may have a weakness in the outer part of the affected disc. Various things may trigger the inner softer part of the disc to prolapse out through the weakened outer part of the disc. For example, sneezing, awkward bending, or heavy lifting in an awkward position may cause some extra pressure on the disc. In people with a weakness in a disc, this may be sufficient to cause a prolapse. Factors that may increase the risk of developing a prolapsed disc include: a job involving lots of lifting, a job involving lots of sitting (especially driving), weight-bearing sports (weight lifting, etc), smoking, obesity, and increasing age (a disc is more likely to develop a weakness with increasing age).
What are the symptoms of a slipped disc?
Back pain: The pain is often severe, and usually comes on suddenly. The pain is usually eased by lying down flat, and is often made worse if you move your back, cough, or sneeze.
Sciatic pain or sciatica: Sciatica is the pain that occurs because a nerve coming from the spinal cord is pressed on (trapped) by a prolapsed disc, or is irritated by the inflammation caused by the prolapsed disc. Although the problem is in the back, you feel pain along the course of the nerve in addition to back pain. Therefore, you may feel pain down a leg to the calf or foot. Sciatic pain can range from mild to severe, but it is often worse than the back pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. The sciatic nerve is a large nerve that is made up from several smaller nerves that come out from the spinal cord in the lower back. It travels deep inside the buttock and down the back of the leg. There is a sciatic nerve for each leg.
Other nerve root symptoms: The irritation or pressure on the nerve next to the spine may also cause pins and needles, numbness or weakness in part of a buttock, leg or foot. The exact site and type of symptoms depend on which nerve is affected.
Cauda equina syndrome: Cauda equina syndrome is a particularly serious type of nerve root problem that can be caused by a prolapsed disc. This is a rare disorder where the nerves at the very bottom of the spinal cord are pressed on. This syndrome can cause low back pain plus: problems with bowel and bladder function (usually unable to pass urine), numbness in the saddle area (around the anus), and weakness in one or both legs. This syndrome needs urgent treatment to preserve the nerves to the bladder and bowel from becoming permanently damaged. See a doctor immediately if you develop these symptoms.
Treatment of slipped disc and sciatic pain
Exercise and keep going: Continue with normal activities as far as possible. This may not be possible at first if the pain is very bad. However, move around as soon as possible, and get back into normal activities as soon as you are able. As a rule, don’t do anything that causes a lot of pain. However, you will have to accept some discomfort when you are trying to keep active.
Medication: If you need painkillers, it is best to take them regularly. This is better than taking them now and again just when the pain is very bad. If you take them regularly the pain is more likely to be eased for much of the time and enable you to exercise and keep active.
– Paracetamol is often sufficient if you take it regularly at full strength. For an adult, this is 1000 mg (usually two 500 mg tablets), four times a day.
– Anti-inflammatory painkillers. Some people find that these work better than paracetamol. They include ibuprofen which you can buy at pharmacies or get on prescription. Other types such as diclofenac or naproxen need a prescription. Some people with asthma, high blood pressure, kidney failure, or heart failure may not be able to take anti-inflammatories.
– A stronger painkiller such as codeine is an option if anti-inflammatories do not suit or do not work well. Codeine is often taken in addition to paracetamol. Constipation is a common side-effect from codeine. This may make back pain worse if you need to strain to go to the toilet. To prevent constipation, have lots to drink and eat foods with plenty of fibre.
– A muscle relaxant such as diazepam is sometimes prescribed for a few days if the back muscles become very tense and make the pain worse.
Ozone Discectomy (Ozonucleolysis): Injection of Ozone-Oxygen mixture into the disc is a new alternative method of treating patients suffering from back and leg pain (sciatica) caused by disc prolapse. Large number of international studies confirms the efficacy of this treatment and superiority of this treatment over conventional disc surgery.
Radiofrequency Ablation: Radiofrequency ablation (or RFA) is a procedure used to reduce pain. An electrical current produced by a radio wave is used to heat up a small area of nerve tissue, thereby decreasing pain signals from that specific area. RFA can be used to help patients with chronic (long-lasting) low-back pain. RFA has proven to be a safe and effective way to treat some forms of pain. It also is generally well-tolerated, with very few associated complications
Surgery: The aim of surgery is to cut out the prolapsed part of the disc. This often eases symptoms. However, it does not work in every case. Also, as with all operations, there is a risk from surgery. It is best to get advise from a qualified doctor regarding the pros and cons of a surgery.
Slipped disc and sciatic pain treatment options available
At NSP clinic, we provide the best and latest non- surgical interventions to treat slipped disc
- Ozone Discectomy (Ozonucleolysis)
- Percutaneous Hydrocision Discectomy
- Endoscopic Discectmy
- Root Sleeve Epidural Injections/Transforaminal injections
- Cervical Epidural Injections
- Facet Blocks
- Radiofrequency Lesioning
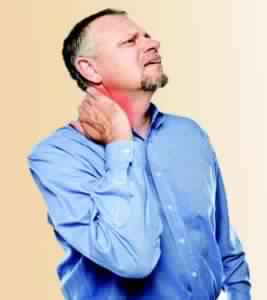
Neck pain (also commonly known as cervical pain, or simply ‘cervical’) is a common problem, with two-thirds of the population having neck pain at some point in their lives. Neck pain affects about 5% population and is more common in women than men. About one-half of episodes resolve within one year but remaining patients continue to suffer pain and associated disability.
Common causes of neck pain and cervical pain
Muscle strains: Overuse and poor posture , such as too many hours hunched over a steering wheel, laptops, mobile phones and other electronic gadgets often triggers muscle strains. Even such minor things as reading in bed or gritting your teeth can strain neck muscles.
Worn Joints: Just like all the other joints in your body, neck joints tend to undergo wear and tear with age, which can cause osteoarthritis in the neck.
Nerve compression: Herniated disks or bone osteophytes (abnormal growth) in the vertebrae of the neck can take up too much space and press on the nerves branching out from the spinal cord.
Injuries: Rear-end automobile collisions often result in whiplash injuries, which occur when the head is jerked backward and then forward, stretching the soft tissues of the neck beyond their limits.
Diseases: Neck pain can sometimes be caused by diseases, such as rheumatoid arthritis, tuberculosis, meningitis or cancer Neck pain can also come from conditions directly affecting the muscles of the neck, such as fibromyalgia
Common Symptoms
- Neck pain is commonly associated with dull aching. Sometimes pain in the neck is worsened with movement of the neck or turning the head. Other symptoms associated with some forms of neck pain include numbness, tingling, tenderness, sharp shooting pain, fullness, difficulty swallowing, pulsations, swishing sounds in the head and dizziness or light-headedness.
- Neck pain can also be associated with headache, facial pain, shoulder pain and arm numbness or tingling (upper extremity paresthesias). These associated symptoms are often a result of nerves getting pinched in the neck. Depending on the condition, sometimes neck pain is accompanied by upper back and/or lower back pain, as is common in inflammation of the spine from ankylosing spondylitis.
When to seek medical advice?
In case of injury, one should seek medical advice immediately without any delay.
If there has not been an injury, you should seek medical care when neck pain becomes:
- Continuous and persistent
- Severe
- Accompanied by pain that radiates down the arms or legs
- Accompanied by headaches, numbness, tingling or weakness
Neck Pain and Cervical Pain Treatment Options
Acute neck pain: Home treatment includes applying heat or ice and using over-the-counter pain relievers. If these modalities don’t show effect, the patient should rush to a pain physician for further detailed evaluation.
Chronic neck pain: If the pain persists or becomes long standing pain then one should not waste any more time and contact a pain physician directly. The treatment options are defined by the exact cause of such a pain. The various options that are available are:
– Physical therapy: Ultrasonic, short wave diathermy, laser and controlled traction. Along with these neck strengthening exercises are performed. No exercises should be performed in acute painful conditions.
– Pharmacotherapy: This includes a combination of nerve medicines, safe pain killers, muscle relaxants and other drugs which are given depending on the exact cause of pain.
– Interventional therapy: If a combination of physical and pharmacotherapy is unable to provide adequate pain relief then we should go for interventional (injection) painmanagement techniques such as cervical epidural and trigger point injections. These techniques are absolutely safe, effective and produce rapid recovery in all age groups provided they are performed by the experts (pain physicians).
– Life style modifications: These are required for prevention of further such events. These include avoiding lifting heavy weights, long uninterrupted work hours in front of laptop, using mobile phones for long periods and use of pillows. Develop good postures while sitting, working, reading, driving etc.
– Surgical options: Surgery is rarely required. There are specific indications for surgery. Presence of pain is not an indication for surgery.
Neck Pain and Cervical Pain Treatment Options available at DPMC
- Physical Therapy
- Cervical Epidural Injection
- Trigger Point Injection
- Facet Injection
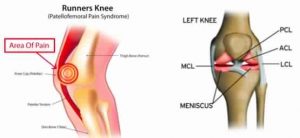
About the Knee
Knee is the largest joint in your body. It is a complex joint made of bone, cartilage and ligaments. The cartilage in the knee acts as a cushion and gliding surface. When healthy, the cartilage keeps the bones in the joint from rubbing together. However, when the joint is affected by arthritis, the bones make contact and cause pain. Injuries, aging and degenerative conditions such as arthritis can cause the cartilage to break down
Common Causes of Knee Pain
Osteoarthritis: Arthritis is a chronic condition that causes joint inflammation. Symptoms include redness, warmth, swelling, tenderness and pain.
Up to 40 percent of the population may have knee osteoarthritis, or “wear and tear” arthritis. This is the gradual breakdown of the cartilage in the knee. Also called degenerative joint disease, osteoarthritis usually develops over years and often is found in patients who have had a knee infection or injury and those who are overweight/
As cartilage wears away, the bones around it can grow thicker and develop bony spurs. This can lead to increased friction between the bones and disrupted movement in your knee. This also can lead to problems with the synovium, a membrane in your knee that produces a liquid to keep your cartilage slippery. This membrane can become inflamed and make too much fluid. This results in swelling, or “water on the knee.” In the most severe cases, the knee can become deformed as the continued friction wears away the bone. Common symptoms of osteoarthritis include pain, stiffness, tenderness, a limited range of motion and a grating sensation when you bend your knee. The pain is usually worse after activity.
Rheumatoid arthritis: Rheumatoid arthritis can affect joints on both sides of the body (both knees, both hands and/or both wrists). In rheumatoid arthritis, your body’s cells attack your own tissues. Rheumatoid arthritis affects three to five times more women than men and often presents between the ages of 20 and 50.
Over time, rheumatoid arthritis can cause cartilage to wear away, swelling in the synovium, and excess fluid in the knee. In later stages, bones can rub against each other.
Bursitis: Bursitis is the inflammation of any of the fluid-filled sacs (bursae) protecting the body’s joints. This is usually caused by repetitive motions or by a stress such as kneeling. Sometimes, a sudden injury can cause bursitis.
Tendonitis: The tendons – rope-like tissues connecting muscles to bone at the knee and other joints – can become painfully inflamed by repetitive and strenuous movement. Tendonitis is a common sports injury, caused by overuse of the same parts of the body. Patellar tendinitis, or “jumper’s knee,” is an inflammation or irritation of the tendon between the knee cap and the shin bone.
Patellofemoral pain syndrome (PFPS): Knee pain or discomfort while walking up and down stairs, jumping or squatting may be symptoms of patellofemoral pain syndrome. This common knee problem is felt toward the front of the knee. It can cause a grinding sensation when bending or straightening your leg, and can cause the knee to occasionally buckle. Sometimes called “runner’s knee,” patellofemoral pain syndrome may be caused by a kneecap that is not aligned properly, overuse, injury, excess weight or when the cartilage in the knee cap is worn significantly.
Injuries: Knee injuries can be the result of sports, falls or trauma. They typically involve the ligaments that hold two of the bones of the knee – the femur and tibia – together eg-ACL,MCL,& Meniscal injuries
How is Knee Pain detected?
A careful medical history which includes
- A description of knee pain (aching, tenderness, burning or swelling)
- Where the pain is located and when it occurs?
- When did the pain start(and if it is the result of an injury or accident )?
- Anything that makes the pain worse or better
Investigations Conducted for Knee Pain
X-rays, MRI, CT Scan
Knee Pain Treatment
Conservative care: Many types of knee pain can be relieved and/ or resolved with conservative treatments such as:
Rest: When the knee is injured or is inflamed, as in bursitis, tendonitis or arthritis, it’s important to rest the joint and avoid overuse. That may mean keeping the knee straight (extended) or in positions that limit bending.
Ice/heat: Applying ice or cold packs to the knee can reduce inflammation and swelling, especially after an injury. Once swelling is gone, heat may be used to help relax and loosen tissues – although ice is the primary treatment.
Pain relievers: Over-the-counter anti-inflammatory medicines can help relieve knee pain, including ibuprofen and naproxen
Weight loss: Lose weight to reduce pressure on the knees.
Braces: In general, knee braces wrap around the knee and leg and help limit unwanted movement while supporting the knee. They are commonly used when knee ligaments are weak, and help to keep the knee from “buckling.”
Injections in the Knee Joint: Potent anti-inflammatory agents can be injected inside the knee to reduce pain and inflammation. Ozone Gas can also be injected into the knee to reduce pain and inflammation. Another nonsurgical injection technique that can provide relief from knee pain is viscosupplementation. This treatment involves injecting a lubricant into the knee. The filler lubricates and adds cushioning to the joint, allowing bones to move more easily and reducing friction. It is a viable solution for mild to moderate OA.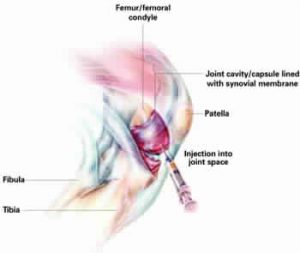
Stem Cell/Platelet Rich Plasma (PRP) therapy: PRP therapy involves injecting platelets from the patient’s own blood to rebuild a damaged tendon or cartilage. It has been successful in not only relieving the pain, but also in jumpstarting the healing process. The patient’s blood is drawn and placed in a centrifuge for 15 minutes to separate out the platelets. The platelet-rich plasma is then injected into the damaged portion of the tendon or cartilage.
Physical therapy: Physical therapies can help you recover from the injury and decrease the pain you are experiencing. They may also include low-impact stretches and exercises that can strengthen muscles in your knee, improve stability and flexibility, and reduce pressure on the joint.
Surgical options: These includes partial and total knee replacements in case of OA or RA knee . In cases of injuries, we can go for arthroscopic or open repair.
Knee Pain Treatment Options available at NSP clinic
- Oral/Physical therapies
- Synvisc-One injections
- Platelet Rich Plasma/Stem Cell therapy
- Intra-articular Ozone Injections
- Radiofrequency lesioning knee joint
Causes of Joint Pain
Joints form the connections between bones. They provide support and help you move. Any damage to the joints from disease or injury can interfere with your movement and cause a lot of pain.
Many different conditions can lead to painful joints, including osteoarthritis, rheumatoid arthritis, bursitis, gout, strains, sprains, and other injuries. Joint pain is extremely common. About one-third of adults report having joint pain within the past 30 days. Knee pain is the most common complaint, followed by shoulder and hip pain, but joint pain can affect any part of your body, from your ankles to your shoulders. As you get older, painful joints become increasingly more common.
Joint pain can range from mildly irritating to debilitating. It may go away after a few weeks (acute), or last for several weeks or months (chronic). Even short-term pain and swelling in the joints can affect your quality of life.
Joint Pain Treatment
Medications: For moderate-to-severe joint pain with swelling, an over-the-counter or prescription nonsteroidal anti-inflammatory drug (NSAID) such as aspirin, or ibuprofen can provide relief. A newer generation of NSAIDs known as Cox-2 inhibitors (Celebrex) is also good for pain relief. If you have milder pain without any swelling, acetaminophen (Tylenol) can be effective. These pain medications should be taken only with the advise of qualified pain physicians. If your pain is so severe that NSAIDs and Cox-2 medicines aren’t effective enough, your pain physician may prescribe a stronger opioid medication.
Physical Therapy: You can work with a physical therapist to strengthen the muscles around the joint, stabilize the joint, and improve your range of motion. The therapist will use techniques such as ultrasound, heat or cold therapy, electrical nerve stimulation, and manipulation.
If you are overweight, losing weight can relieve some of the pressure on your painful joints. Exercise is one effective way to lose weight (along with diet), but be careful to stick with low-impact exercises that won’t further irritate the joint. Swimming and bicycling are among the best exercises because both allow you to exercise your joints without putting impact on them. Because water is buoyant, swimming also relieves some of the pressure on your joints.
Home Care: You can relieve short-term joint pain with a few simple techniques at home. Some of these tips include:
- Protecting the joint with a brace or wrap.
- Resting the joint, avoiding any activities that cause you pain.
- Applying ice on the joint for about 15 minutes, several times each day.
- Compressing the joint using an elastic wrap.
- Elevating the joint above the level of your heart.
Applying ice to your painful joints can relieve the pain and inflammation. For muscle spasms around joints, try using a heating pad or wrap several times a day.
Injections: Potent anti-inflammatory agents can be injected into the joints to reduce pain and inflammation. Ozone Gas injections have also clinically proven to be extremely effective at pain relief.
Other injection options include:
- Removing fluid from the joint (and is often done in connection with a steroid injection)
- Injections of hyaluronan, a synthetic version of the natural joint fluid. This is used to treat osteoarthritis
Stem Cell/Platelet Rich Plasma (PRP) therapy: PRP therapy involves injecting platelets from the patient’s own blood to rebuild a damaged tendon or cartilage. It has been successful in not only relieving the pain, but also in jumpstarting the healing process. The patient’s blood is drawn and placed in a centrifuge for 15 minutes to separate out the platelets. The platelet-rich plasma is then injected into the damaged portion of the tendon or cartilage.
Surgery: Surgery procedures (like Total Hip Replacement) are used as a last resort. Like all other surgeries, these surgeries have their own issues like associated risks and high hospitalization and recovery times. Even then, the success rate for surgeries is limited to 60-70%.
Joint Pain Treatment options available at DPMC
- Oral/Physical therapies
- Synvisc-One injections
- BOTOX injections
- Platelet Rich Plasma/Stem Cell therapy
- Intra-articular Ozone Injections
Arthritis is a condition that affects more than 10% of the adult population. There are more than 100 different types of arthritis. The false notion that all arthritis is alike has led people to try treatments that have little effect on their arthritis symptoms. Since each type of arthritis is different, each type calls for a different approach to treatment. That means an accurate diagnosis is crucial for anyone who has arthritis.
What Are the Common Types of Arthritis?
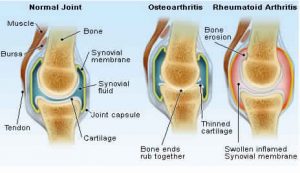
There are two major types of arthritis — osteoarthritis, which is the “wear and tear” arthritis, and rheumatoid arthritis, an inflammatory type of arthritis that happens when the body’s immune system does not work properly. Gout, which is caused by crystals that collect in the joints, is another common type of arthritis. Psoriatic arthritis, lupus, and septic arthritis are other types.
Osteoarthritis
Osteoarthritis is also called degenerative joint disease or degenerative arthritis. It is the most common chronic joint condition. Osteoarthritis results from overuse of joints but most commonly it is an aging phenomenon. It can be the consequence of demanding sports where joints may be injured or obesity, which places increased load on weight bearing joints. Osteoarthritis in the hands is frequently inherited and often happens in middle-aged women. Osteoarthritis is most common in joints that bear weight — such as the knees, hips, feet, and spine. It often comes on gradually over months or even years. Except for the pain in the affected joint, you usually do not feel sick, and there is no unusual fatigue or tiredness as there is with some other types of arthritis.
With osteoarthritis, the cartilage gradually breaks down. Cartilage is a slippery material that covers the ends of bones and serves as the body’s shock absorber. As more damage occurs, the cartilage starts to wear away, or it doesn’t work as well as it once did to cushion the joint. As an example, the extra stress on knees from being overweight can cause damage to knee cartilage. That, in turn, causes the cartilage to wear out faster than normal.
As the cartilage becomes worn, cushioning effect of the joint is lost. The result is pain when the joint is moved. Along with the pain, sometimes you may hear a grating sound when the roughened cartilage on the surface of the bones rubs together. Painful spurs or bumps may appear on the end of the bones, especially on the fingers and feet. While not a major symptom of osteoarthritis, inflammation may occur in the joint lining as a response to the breakdown of cartilage.
Symptoms of osteoarthritis, depending on which joint or joints are affected, may include:
- Deep, aching pain
- Difficulty dressing or combing hair
- Difficulty gripping objects
- Difficulty sitting or bending over
- Joint being warm to the touch
- Morning stiffness for less than an hour
- Pain when walking
- Stiffness after resting
- Swelling of joint
- Loss of motion in a joint
Rheumatoid Arthritis
Rheumatoid arthritis is the most common type of inflammatory arthritis. About 75% of those affected are women. In fact, between 1% and 3% of women are likely to develop rheumatoid arthritis in their lifetime.
Rheumatoid arthritis is an autoimmune disease. That means that the immune system attacks parts of the body. The joints are the main areas affected by this malfunction in the immune system. Over time, chronic inflammation can lead to severe joint damage and deformities. About one out of every five people who have rheumatoid arthritis develop lumps on their skin called rheumatoid nodules. These often develop over joint areas that receive pressure, such as over knuckles, elbows, or heels.
Symptoms of rheumatoid arthritis can come on gradually or start suddenly. Unlike osteoarthritis, symptoms of rheumatoid arthritis are often more severe, causing pain, fatigue, loss of appetite, stiffness.
With rheumatoid arthritis, you may feel pain and stiffness and experience swelling in your hands, wrists, elbows, shoulders, knees, ankles, feet, jaw, and neck. Sometimes the pain occurs in one body part. But more commonly, rheumatoid arthritis pain occurs in combinations of several joints such as in the hands, knees, and feet.
With rheumatoid arthritis, the joints tend to be involved in a symmetrical pattern. That is, if the knuckles on the left hand are inflamed, the knuckles on the right hand will also be inflamed. After a period of time, more of your joints may gradually become involved with pain and swelling and may feel warm to the touch. The joint swelling is persistent and interferes with activities. For example, it can interfere with opening a jar, driving, working, and walking — the very activities that allow us to function in our daily lives.
Arthritis Pain Treatment
Medication: Over-the-counter (OTC) medications for pain relief, like acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen sodium, provide relief from arthritis pain. OTC acetaminophen can reduce mild and moderate arthritis pain that often accompanies osteoarthritis.
In addition to medications, there are supplements and creams that you can purchase over the counter that may also alleviate arthritis pain.
Among the most popular supplements used by people with osteoarthritis are glucosamine and chondroitin. In those with moderate to severe knee pain from osteoarthritis, the combination of glucosamine and chondroitin sulfate may be effective in providing pain relief, although medical studies have not shown clear proof that they are helpful in everyone.
In addition to over-the-counter NSAID medications, pain physicians can suggest prescription NSAIDs to treat arthritis pain and inflammation. Prescription NSAIDs may also be available in topical and injectable forms. Besides ibuprofen and naproxen, other examples of prescription NSAIDs include diclofenac and others.
Injections: Potent anti-inflammatory agents (like Synvisc One) can be injected to reduce pain and inflammation. Ozone Gas injections have also clinically proven to be extremely effective at pain relief.
Stem Cell/Platelet Rich Plasma (PRP) therapy: PRP therpay involves injecting platelets from the patient’s own blood to rebuild a damaged tendon or cartilage. It has been successful in not only relieving the pain, but also in jumpstarting the healing process. The patient’s blood is drawn and placed in a centrifuge for 15 minutes to separate out the platelets. The platelet-rich plasma is then injected into the damaged portion of the tendon or cartilage.
Surgery: Surgery procedures are used as a last resort. Like all other surgeries, these surgeries have their own issues like associated risks and high hospitalization and recovery times. Even then, the success rate for surgeries is limited to 60-70%.
Arthritis Pain Treatment available at DPMC
- Physical therapy
- Lifestyle modification advice and counseling
- Intraarticular Synvisc-One injection
- Intraarticular ozone injection
- BOTOX injection
- Platelet Rich Plasma (PRP) therapy
What is Cerebral Palsy?
Cerebral palsy (CP) is a physical disability that affects movement and posture. CP refers to a group of disorders affecting a person’s ability to move. It is a permanent life-long condition, but generally does not worsen over time. It is due to damage to the developing brain either during pregnancy or shortly after birth
Cerebral palsy affects people in different ways and can affect body movement, muscle control, muscle coordination, muscle tone, reflex, posture and balance.
People who have cerebral palsy may also have visual, learning, hearing, speech, epilepsy and intellectual impairments.
Cerebral Palsy Treatment
A variety of treatments can help people who have CP to make the most of their abilities and physical strength, prevent complications, and improve their quality of life.
Specific treatment varies by individual and changes as needed if new issues develop. In general, treatment focuses on ways to maintain or improve a person’s quality of life and overall health.
Regular visits with your pain physician are important for monitoring your child’s condition.
Treatment for CP includes:
Physiotherapy: Physiotherapy is an important part of managing CP. It usually starts soon after diagnosis. It may begin earlier, depending on the symptoms. Some people with CP continue physiotherapy throughout their lives, especially those with severe physical disabilities.
The goals of physiotherapy are to:
- Foster independence by improving functional mobility
- Strengthen and encourage the growth of muscles.
- Improve the ability to move all parts of the body
- Prevent joints from becoming tight or permanently bent (contracted)
BOTOX Injections for CP treatment: Botulinum Toxin (BOTOX) Type A is a muscle relaxant derived from the bacterium Clostridium Botulinum. In controlled doses, it can provide safe, effective relief from a number of conditions. BOTOX has been successfully used to treat CP and other muscular conditions in children and adults for over 20 years. Clinical studies and trials have indicated positive and helpful results.
Nerve Blocks: Nerve blocks using phenol in the foot and ankle has clinically proven to be effective in providing relief from CP.
Cerebral Palsy Treatment Options available at DPMC
- Physiotherapy
- BOTOX injections for cerebral palsy treatment
- Nerve blocks
Heel Pain
Causes of Heel Pain
Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Pain Beneath the Heel
If it hurts under your heel, you may have one or more conditions that inflame the tissues on the bottom of your foot:
Plantar fasciitis: One of the most common causes of heel pain is plantar fascitiis. This is causes due to the inflamaation of the band of tissue connecting the heel bone to the toes. Pain due to plantar fasciitis can be gelt in the heel or the arch and is usually worst in the morning. The first step coming out of bed is usually the most painful one. Common causes of plantar fasciitis include high level of physical activity; standing for prolonged periods on concrete or hard surfaces; faulty foot mechanics like flat-feet; tight calf muscles; increased weight; and improper footwear. It is a condition commonly seen in distance runners, but is also extremely common in the general population.
Heel spur: When plantar fasciitis continues for a long time, a heel spur (calcium deposit) may form where the fascia tissue band connects to your heel bone. Having a heel spur may not cause pain and should usually not be operated.
Stone bruise: When you step on a hard object such as a rock or stone, you can bruise the fat pad on the underside of your heel. It may or may not look discolored. The pain goes away gradually with rest.
Pain Behind the Heel
If you have pain behind your heel, this may be due to the inflammation of the area where the Achilles tendon meets the heel bone. This may happen due to too much running or wearing sheos that rub the heel too much. Such pain typically builds slowly over time, and the skin becomes thick, red and swollen, in this process.
Retrocalcaneal buritis: The bursa acts as a lubricant when muscles/tendons slide over bones. Bursas exist around most large joints of the body, including the ankle.
The bursa located at the back of the ankle, by the heel, is called retrocalcaneal bursa. Repeated/excessive use of the ankle may cause the bursa to get inflamed, leading to this condition called retrocalcaneal bursitis.
The most common symptoms of retrocalcaneal bursitis include:
- Pain in the heel, especially with walking, running, or on touching the heel
- Increased pain when standing on tiptoes
- Red, warm skin over the back of the heel
Achilles Tendonitis: Achilles tendon connects the calf muscle to the heel. This tendon is used for walking, running and jumping. Achilles tendonitis is a condition in which this tendon gets inflamed due to uveruse of the foot. This condition is most common in people below 35 years of age, and often occurs in runners and other athletes.
Symptoms include pain in the heel and along the length of the tendon when walking or running. The tendon may be painful to touch or move. The area may become swollen, and you may have trouble standing up on one toe.
Achilles tendonitis is more likely to occur in cases of:
- Sudden increase in activity
- Running on hard surfaces
- Excessive running
- Excessive jumping (for example, when playing basketball)
- Wearing improper shoes
Ankle Pain
Causes of Ankle Pain

Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Ankle Sprains: An ankle sprain is an injury to the bands of ligaments that surround and connect the bones of the leg to the foot. The injury typically happens when you accidentally twist or turn your ankle in an awkward way. This can stretch or tear the ligaments that hold your ankle bones and joints together.
Rheumatoid Arthritis (RA): RA is a chronic disease of the joints that occurs when the body’s immune system mistakenly attacks the synovium, the thin membrane that lines the joints. The result can be joint damage, pain, swelling, inflammation, loss of function and disability. In about 90% patients with rheumatoid arthritis, the joints of the feet are ankles are affected.
Gout: Gout is a form of arthritis that occurs when excess uric acid, a bodily waste product circulating in the bloodstream, is deposited as needle-shaped monosodium urate crystals in tissues of the body, including the joints. For many people, the first symptom of gout is excruciating pain and swelling in the big toe – often following a trauma, such as an illness or injury. Subsequent attacks may occur off and on in other joints, including the ankles. After years with the disease, lumps of uric acid, called tophi, may form beneath the skin around the ankles.
Prevention of Heel & Ankle Pain
To prevent ankle/heel pain, ensure the following:
- Perform proper warm-up before running, exercise, sports, or any other strenuous activity.
- Maintain ideal body weight
- Wear supportive footwear whenever bearing weight (for example, have supportive shoes placed near bedside to put on before taking initial steps)
Treatment of Heel & Ankle Pain
There are a number of treatment modalities that can help relieve heel and annkle pain and speeden up your recovery. These include:
Conservative Care
Resting your heel: Try to avoid walking long distances and standing for long periods
Fomentation: Alternate hot and cold fomentation helps reduce pain and swelling
Regular stretching: Stretching your calf muscles and plantar fascia helps reduce pain
Correct shoes: Wearing good-fitting shoes that support and cushion your foot – running shoes are particularly useful.
Medication and Pharmacotherapy
One of the easiest techniques for pain control is using an icepack on the affected heel and taking painkillers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and adding a neuropathic agent in case of prolongation of pain.
Braces and supportive devices
Using supportive devices such as orthoses (rigid supports you put inside your shoe) or strapping can help control pain in the ankle and heel.
Interventional techniques
Intralesional injections in the ankle & heel have been found to provide significant pain relief in cases where medicines haven’t worked. Such interventional techniques should be followed by regular stretching and exercises for better results.
Platelet Rich Plasma (PRP) Therapy
A more recent technique used for heel and ankle pain, PRP has become one of the most preferred minimally invasive technique for treating pain in the heel and ankle. At Delhi Pain Management, PRP has been used in over 500 cases of heel and ankle pain, with very positive results.
PRP therapy involves injecting platelets from the patient’s own blood to rebuild a damaged tendon or cartilage. It has been successful in not only relieving the pain, but also in jumpstarting the healing process. The patient’s blood is drawn and placed in a centrifuge for 15 minutes to separate out the platelets. The platelet-rich plasma is then injected into the damaged portion of the tendon or cartilage.
Heel & Ankle Pain Treatment Options Available at DPMC
At DPMC, we provide the best and latest non- surgical interventions to treat heel and ankle pain
- Medication/Supporting braces
- Injections in the Heel & Ankle
- Platelet Rich Plasma Therapy
- Physiotherapy
What is migraine?
Migraine is a condition that causes attacks (episodes) of headaches. Other symptoms such as feeling sick (nausea) or being sick (vomiting) are also common Between migraine attacks, the symptoms go completely.
Who gets migraine?
Migraine is common. About 1 in 4 women and about 1 in 12 men develop migraine at some point in their lives. It most commonly first starts in childhood or as a young adult. Some people have frequent attacks – sometimes several a week. Others have attacks only now and then. Some people may go for years between attacks. In some people, the migraine attacks stop in later adult life. However, in some cases the attacks continue (persist) throughout life.
What are the types and symptoms of migraine?
There are two main types of migraine attack:
Migraine attack without aura (also called common migraine): This is the most common type of migraine. Symptoms include the following:
- The headache is usually on one side of the head, typically at the front or side Sometimes it is on both sides of the head Sometimes it starts on one side, and then spreads all over the head The pain is moderate or severe and is often described as throbbing or pulsating Movements of the head may make it worse It often begins in the morning, but may begin at any time of the day or night Typically, it gradually gets worse and peaks after 2-12 hours, then gradually eases off However, it can last from 4 to 72 hours
- Other migraine symptoms that are common:
- Feeling sick (nausea)
- Being sick (vomiting)
- Not liking bright lights or loud noises, so that you may just want to lie in a dark room
- Other symptoms that sometimes occur:
- Being off food
- Blurred vision
- Poor concentration
- Stuffy nose
- Hunger
- Diarrhoea
- Tummy (abdominal) pain
- Passing lots of urine
- Going pale
- Sweating
- Scalp tenderness
- Sensations of heat or cold
Migraine attack with aura (also called classic migraine): About 1 in 4 people with migraine have migraine with aura. The symptoms are the same as those described above (migraine without aura), but also include a warning sign (an aura) before the headache begins.
Visual aura is the most common type of aura. Examples include a temporary loss of part of vision, flashes of light, objects may seem to rotate, shake, or boil. Numbness and pins and needles are the second most common type of aura. Numbness usually starts in the hand, travels up the arm, then involves the face, lips, and tongue. The leg is sometimes involved. Problems with speech are the third most common type of aura. Other types of aura include an odd smell, food cravings, a feeling of well-being, other odd sensations.
One of the above auras may develop, or several may occur one after each other. Each aura usually lasts just a few minutes before going, but can last up to 60 minutes. The aura usually goes before the headache begins. The headache usually develops within 60 minutes of the end of the aura, but it may develop a lot sooner than that – often straight afterwards.
How is migraine diagnosed? Do I need any tests?
Migraine is usually diagnosed by the typical symptoms. There is no test to confirm migraine. A doctor can usually be confident that you have migraine if you have typical symptoms and by an examination which does not reveal any abnormality.
What causes migraine?
The cause for migraines is not clear. It was believed blood vessels in parts of the brain become narrower (go into spasm) which accounted for the aura. The blood vessels were then thought to open wide (dilate) soon afterwards, which accounted for the headache. It is now thought that some chemicals in the brain increase in activity and parts of the brain may then send out confusing signals which cause the symptoms.
Migraine treatment
Medication: Paracetamol or aspirin works well for many migraine attacks. Take a dose as early as possible after symptoms begin. If you take painkillers early enough, they often reduce the severity of the headache, or stop it completely. A lot of people do not take a painkiller until a headache becomes really bad. This is often too late for the painkiller to work well.
Anti-inflammatory painkillers probably work better than paracetamol. They include ibuprofen and aspirin.
Injections: For treating chronic migraines and headaches, injections like the Occipital nerve block and Sphenopalatine ganglion block have proven to be effective. BOTOX® injections are the first and only FDA-approved preventive treatment proven to reduce migraine and headache days every month.
Migraine treatment & Headache treatment options available at DPMC
- BOTOX injection
- Occipital nerve block
- Sphenopalatine ganglion block
Neuralgia is a stabbing, burning, and often quite severe pain that occurs along a damaged nerve. The damaged nerve may be anywhere in the body, but is most common in the face and neck. The cause of a damaged nerve may be a disease like diabetes (diabetic neuropathy) or multiple sclerosis, an infection like shingles, or the result of old age. Treatment for the pain of neuralgia depends on the cause.
Types of Neuralgia
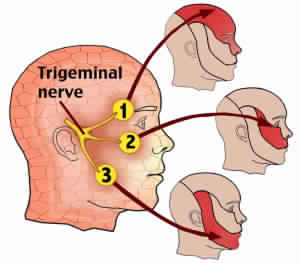
Neuralgia can occur in different parts of the body and can have various causes.
Trigeminal Neuralgia: This type of neuralgia is associated with pain from the trigeminal nerve, which goes from the brain to the face. The particular cause of pain is believed to be a blood vessel pressing down on the trigeminal nerve where it meets with the brainstem. Trigeminal neuralgia causes pain in the face, usually on one side, and is most common in the elderly.
Postherpetic Neuralgia: This type of neuralgia occurs as a complication of shingles and may be anywhere on the body. Shingles is a viral infection characterized by a painful rash and blisters. Neuralgia can erupt wherever the outbreak of shingles occurred and can be mild or severe, persistent or intermittent, and can last for months or years.
Glossopharyngeal Neuralgia: Pain from the glossopharyngeal nerve, which is in the throat, is not very common. This type of neuralgia produces pain in the neck and throat.
Causes of Neuralgia
The underlying cause of any type of neuralgia is damage to a nerve. Each nerve in your body is protected by a coating called the myelin sheath. When the myelin is damaged or wears away from the nerve, the stabbing, severe, shock-like pain of neuralgia results. There are many different factors, including old age, which can cause damage to the myelin. Unfortunately, in many cases of neuralgia, a cause can never be found.
Infection: The cause of postherpetic neuralgia is shingles, an infection caused by the chickenpox virus. The likelihood of having this infection increases with age. Lyme disease, HIV, and syphilis can also cause neuralgia.
Multiple Sclerosis: Multiple sclerosis (MS) is a disease that is caused by the degradation of myelin. Among the many symptoms that result from MS is neuralgia, often in the face.
Pressure on Nerves: The myelin on nerves can be worn away by pressure. The pressure may come from a bone, ligament, blood vessel, or a tumor that is pressing on the nerve. The pressure of a swollen blood vessel is a common cause in trigeminal neuralgia.
Diabetes (Diabetic Neuropathy): Many people with diabetes will suffer from some type of neuralgia because excess glucose in the bloodstream can lead to myelin damage.
Less Common Causes: If the cause of neuralgia cannot be blamed on an infection, MS, diabetes, or pressure on the nerves, it may be from one of many less common factors. These include:
- chronic kidney disease
- porphyria (a rare blood disease)
- medications like cisplatin, paclitaxel, or vincristine (prescribed to cancer patients)
- trauma, such as that caused by surgery
- chemical irritation
Neuralgic Pain Treatment Options
Medications: Medicines can be used to relieve neuropathic pain. Medications prescribed may include:
- over-the-counter pain relievers like aspirin or ibuprofen
- antidepressants
- anti-seizure medications
- topical creams with capsaicin
Nerve Blocks: Nerve blocks (like trigeminal nerve block) are injections directed at a particular nerve or nerve group that is intended to reduce inflammation and relieve pain
Chemical Neurolysis (Alcohol / Phenol Injections): Alcohol or Phenol injections are commonly used for bringing substantial relief in trigeminal neuralgia
Radiofrequency Ablation: RF ablation is commonly used in trigeminal neuralgia to numb the pain-generating structure and reduce the intensity of pain.
Neuralgic Pain Treatment Options available at NSP clinic
- Physical therapy and lifestyle modification counseling
- Medication
- Nerve blocks
Sports injuries
refers to a broad category of injuries in various parts of the body, which can be caused due to strenuous activities, such as sports. There are certain parts of the body that are more prone to damage from sports injuries. Below are the top 8 most common types of sports injuries. The top three categories (Runner’s Knee, Shoulder Injury, and Ankle Sprain) comprise more than 80% of all sports injuries.
- Runner’s Knee: Runner’s knee is the most common type of sports injury. The problem happens most commonly to runners, cyclists, swimmers, as well as people who practice aerobics, play football, basketball and volleyball. Overuse of the knee leads to irritation of the tendon below the knee-cap which results in this problem.
- Knee Ligament Injuries (ACL Tear/MCL Tear/PCL Tear/Meniscus Tear): Knee injuries can be the result of getting hit on the knee, falling down, or landing on a flexed knee. These are most common to footballers. These typically involve the ligaments that hold two of the bones of the knee – the anterior cruciate ligament (ACL), the medial cruciate ligament (MCL), or the posterior cruciate ligament (PCL).
- Shoulder Injury (Rotator Cuff Tear): These injuries occur mostly during tennis, swimming, and voleyball. The chief cause of these problems is the overuse of the shoulder, which loosens the rotator cuff (a group of tendons and muscles around the shoulder).
- Ankle Sprain: Ankle sprains are common to any activity that involves jumping, running or turning quickly (e.g., playing football, basketball etc). Such motion can lead to twisting of the ankle and possible tearing of a tendon/ligament.
- Tennis/Golfer’s Elbow: Tennis Elbow involves tendon degeneration in the elbow due to repeated backhand strokes common to tennis. This condition leads to pain on the outside of the elbow. Golfers Elbow impacts the inside of the elbow, due to the inflammation of the muscles responsible for forearm-flexing.
- Shin Splints: Shin Splints refers to pain on the inside of shinbone caused by inflammation of the surrounding muscles. These occur mostly in cases of inactive people
who start working out and increase their intensity too fast. - Groin Strain: This refers to a strain the adductor muscles, situated in the upper thigh which help to pull the legs together and causes sharp pain and swelling on the inside of the thigh. This usually happens when one changes directions suddenly while running.
- Hamstring Strain: The hamstrings are the muscles behind your thighs. Hamstring strains most commonly occur due to inadequate warming up or excessive fatigue.
Prevention of Sports Injuries
- One of the easiest, yet most important prevention technique for sport injuries is to choose the correct shoes and insoles, and keep replacing them regularly as they get worn out.
- Running on a softer surface like an indoor track rather than the road or pavement can also prevent a number of injuries.
- To prevent shoulder injuries, it is most important to strengthen your muscles through weight training before getting involved in active sports.
- Always stretch properly before and after exervise, and do not work out when you are weak or fatigued.
- Never resume your sports activities until your injury is fully healed. Restarting activiity too soon can lead to chronic issues.
Treatment of Sports Injuries
Medicines/Pharmacotherapy: One of the easiest techniques for pain control is using conservative care (e.g., resting the impacted part, using hot/cold packs) along with medicines, such as Nonsteroidal anti-inflammatory drugs (NSAIDs) and adding a neuropathic agent in case of chronification of pain.
Braces: Depending on the site of injury, different braces (e.g., thigh brace, elbow brace, arch brace, wrist brace, ankle brace, or knee brace) can be used to restrict the motion of the impacted part, control pain and speed up the recovery process.
Injections: Intralesional injections in the impacted part can provide significant pain relief in cases where medicines haven’t worked. Such interventional techniques should be followed by regular stretching and exercises for better results.
Platelet Rich Plasma (PRP) Therapy: PRP therapy involves injecting platelets from the patient’s own blood to rebuild a damaged tendon or cartilage. It has been successful in not only relieving the pain, but also in jumpstarting the healing process. The patient’s blood is drawn and placed in a centrifuge for 15 minutes to separate out the platelets. The platelet-rich plasma is then injected into the damaged portion of the tendon or cartilage.
PRP has been successfully used at NeuroSpineAndPain Clinic for several different types of sports injury conditions, such as golfer’s elbow, tennis elbow, shoulder injury, and knee ligament tears (ACL tear, PCL tear, meniscus tear).
Sports Injuries Treatment Options Available at NSP clinic
At NSP clinic, we provide the best and latest non- surgical interventions to treat pain due to sports injuries
- Medication/Supporting braces
- Injections
- Platelet Rich Plasma Therapy
- Physiotherapy
FIBROMYALGIA
What is Fibromyalgia?
Fibromyalgia is an increasingly recognized chronic pain illness which is characterized by widespread musculoskeletal aches, pain and stiffness, soft tissue tenderness, general fatigue and sleep disturbances. The most common sites of pain include the neck, back, shoulders, pelvic girdle and hands, but any body part can be involved.
Causes of Fibromyalgia
The exact cause of this condition is not known. However, the pain pathways, hormonal changes and immune system disturbances have all been studied and found in patients with fibromyalgia. This suggests a deeper and multifactorial causation of the condition.
Diagnosis of Fibromyalgia
The condition may often be a challenge to diagnose. This is because there are no clear cut sensitive tests that diagnose the condition with conviction. Much of the diagnosis is based on detailed examination of the patient and presence of symptoms.
Top Ten Fibromyalgia Symptoms
- Pain all over the body > 3months duration
- Day time tiredness/Fatigue
- Sleep difficulties
- Brain fog/depression
- Morning stiffness
- Muscle knots, cramping, weakness
- Irritability/anger
- Headaches/migraines
- Short term memory loss
- Presence of multiple tender points
Fibromyalgia Facts
- Affects 7-8 percent of the general population
- Occurs in people of all ages, even children
- More common in women, although men develop fibromyalgia too
- Symptoms are chronic but may fluctuate throughout the day
- Roughly 25% of people with fibromyalgia are work-disabled
- Three drugs are FDA-approved for fibromyalgia treatment
- Fibromyalgia is Manageable with medications and exercises
Fibromyalgia Treatment
The mainstay of treatment is physical therapy. Optimal physical therapy can only be carried out once adequate pain relief is achieved. Adequate pain relief can be achieved by a combination of nerve medicines to quieten the nerves and safe pain killers, which are continued for longer periods of time.
Tips to help relieve Fibromyalgia pain
You can manage your pain by a simply understanding the disease and realising the importance of lifestyle modifications. A long-term commitment has to be made to improve your quality of life .The wellness approach to fibromyalgia includes:
Alteration of daily activities/Lifestyle modifications: Maintaining a proper posture during sitting, standing, work and sleep are important to minimise muscle stiffness. Managing stress and pacing your daily activities will help your overall well being.
Exercises: An exercise programme that includes stretching of muscles and mobility of all joints of the body is started. You can even start with just 5 minutes a day approach with either gentle walks or stretching exercises. This can gradually be increased to 15-20 minutes every day. Proper rest should also be a part of your daily programme. Aerobic exercises can also be a part of your treatment once the pain has reduced considerably.
Swimming/Aquatic Therapy: Swimming or hydrotherapy can help relieve muscle stiffness and improving flexibility of muscles. Regular swimming can go a long way in improving your quality of life.
Yoga: Regular yoga exercises can help in relaxing stiff muscles and achieving flexibility of the body. Yoga results in both relief of pain as well as relaxation of mind.
Maintaining a regular sleep/wake cycle: A regular 6-8 hours sleep is essential to minimise the fatigue and stiffness of muscles.
Therapy: Massage, ultrasound, vibrations and other muscle strengthening therapies including electrical nerve stimulation can help you in relaxing muscles and release pain. Pharmacological agents (medicines) prescribed by your doctor will also help in getting ready to start your daily exercises and work routine.
OSTEOPOROSIS
What is Osteoporosis?
Osteoporosis is a condition marked by decreased bone density, which results in lower bone strength and higher fragility. In this condition, bones become abnormally porous and compressible, like a sponge.
Osteoporosis greatly weakens the bones and results in frequent fractures. These fractures typically occur in the hip, wrist or spine.
What is Osteopenia?
Osteopenia is a bone condition where the density reduces slightly. The density in this condition is lesser than a normal bone but not as less as osteoporosis. Osteopenia often leads to osteoporosis, when left unchecked.
Symptoms of Osteoporosis
A person is often not aware that he or she has osteoporosis until a fracture occurs. But there are occasionally symptoms of the disorder. They could include:
- Backache
- A gradual loss of height and an accompanying stooped posture
- A stooped posture
What causes Osteoporosis?
Most factors that govern your risk of osteoporosis are outside your control. For example, women are much more likely to develop osteoporosis. Also, the risk of osteoporosis increases with age. Besides these uncontrollable factors, controllable reasons like dietary factors and intake of certain medicines are also associated with osteoporosis. For example, low calcium intake or general eating disorders greatly increase the risk of osteoporosis.
Diagnosis of Osteoporosis
A simple test which is commonly available called Bone Mineral Density (BMD) Measurement can help detect the presence of osteopenia or osteoporosis.
Treatment of Osteoporosis
Medication and Pharmacotherapy: In osteopenia and early-stage osteoporosis, oral medicines are the most common treatment to control the problem.These medicines fall under the category of bisphosphonates. Examples of these medicines include Alendronate, Risedronate and Ibandronate.
Intravenous infusions of Zoledronic Acid: In more severe cases of osteoporosis, it becomes important to take more urgent action through intravenous infusions of medicines, like Zoledronic Acid.
Osteoporosis Treatment Options Available at NSP clinic
At NSP clinic, we provide the best and latest non- surgical interventions to control osteoporosis
- Medications
- Intravenous infusions (zoledronic acid)
CANCER PAIN
Causes of Cancer Pain
Most cancer pain is caused by the tumour pressing on bones, nerves or other organs in your body. Sometimes pain is related to your cancer treatment. For example, some chemotherapy drugs can cause numbness and tingling in your hands and feet or a burning sensation at the place where they are injected. Radiotherapy can cause skin redness and irritation.
Remember that some pain may have nothing to do with your cancer. You may have the general aches and pains that everyone gets from time to time.
Types of Cancer Pain
Cancer pain can be acute or chronic. Acute pain is due to damage caused by an injury and tends to only last a short time. For example, having an operation can cause acute pain. The pain goes when the wound heals. In the meantime, painkillers will usually keep it under control.
Chronic pain is pain caused by changes to nerves. Nerve changes may occur due to cancer pressing on nerves or due to chemicals produced by a tumour. It can also be caused by nerve changes due to cancer treatment. The pain continues long after the injury or treatment is over and can range from mild to severe. It can be there all the time and is also called persistent pain. Chronic pain can be difficult to treat, but painkillers or other pain control methods can successfully control it in about 95 out of every 100 people.
The amount of pain you have with cancer depends on
- The type of cancer you have
- Where it is
- The stage of your cancer
- Whether the cancer or treatment has damaged any nerves
- Other factors such as fear, anxiety, depression and a lack of sleep can also affect how you feel pain.
If you have pain it is very important to let your pain physician know straight away. If you try to put up with the pain, this can lead to nerve changes that may make the pain harder to control in the future
Cancer Pain Treatment
Oral Medications: Painkilling drugs work to control cancer pain in most people. The key to controlling cancer pain is to take your medicine on a regular schedule. Do not wait until your pain gets bad. Pain is easier to control when you treat it just after it starts.
Be careful when taking nonprescription medicines. Talk with a pain physician before you take these medicines, especially if you have a fever or have had kidney or liver disease, gastrointestinal bleeding, or a stomach ulcer. Prescription medicines may be used alone or with other medicines. Depending on your pain, some of these medicines work better than others. Prescription medicines include:
- Opiate pain relievers, such as fentanyl, hydromorphone, methadone, morphine, oxycodone, and tramadol.
- Other medicines that may be used with opiate pain relievers. These medicines may be given to help your pain medicine work better or to treat your symptoms. Or they may be given for certain types of pain. These include:
- Anticonvulsants, to help control nerve pain like burning and tingling.
- Antidepressants, to relieve pain and help you sleep.
- Anti-inflammatory drugs and corticosteroids (for example, prednisone or dexamethasone).
- Bisphosphonates, such as pamidronate and zoledronic acid, to treat bone pain.
- Local anesthetics, such as skin creams with capsaicin or lidocaine, to help relieve pain in the skin and surrounding tissues.
Nerve Blocks: Nerve blocks are injections containing potent anti-inflammatory agents directed at a particular nerve or nerve group that is intended to reduce inflammation and relieve pain.
Intrathecal Pump: Also called infusion pain pumps or spinal drug delivery systems. In this procedure, a pocket is made under the skin that’s large enough to hold a medicine pump. The pump is usually about one inch thick and three inches wide. A catheter is also inserted, which carries pain medicine from the pump to the intrathecal space around the spinal cord. The implants deliver medicines directly to the spinal cord, where pain signals travel. For this reason, intrathecal drug delivery can provide significant pain control with a fraction of the dose that would be required with pills. In addition, the system can cause fewer side effects than oral medications because less medicine is required to control pain.
Radiofrequency Ablation ( RFA) is a procedure used to reduce pain. An electrical current produced by a radio wave is used to heat up a small area of nerve tissue, thereby decreasing pain signals from that specific area. RFA can be used to help patients with chronic (long-lasting) cancer pain. RFA has proven to be a safe and effective way to treat some forms of pain. It also is generally well-tolerated, with very few associated complications.
Cancer Pain Treatment options available at NSP clinic
- Oral medications
- Oral morphine therapy
- Psychological and lifestyle counseling
- Fentanyl patches
- Nerve blocks
- Intrathecal pumps
