
SCOLIOSIS
What is Spinal Deformity Reconstruction?
There are many reasons for spine to misshapen, because of scoliosis, kyphosis, Scheuermann’s disease and other problems. In such spinal deformity patients, the spine is curved from side to side, rotated and/or curved forward too much. There are many ways to reconstruct a curved spine. The type of surgery for spinal reconstruction depends on the degree of the curve, where the curve is located within the spine, patient age, patient general health and other factors. Spinal reconstruction generally involves the use of screws, hooks or wires that grasp or attach to the vertebral bodies. The curve is then straightened as much as possible by attaching a rod to the attachment points. Sometimes an interbody fusion (fusion between the vertebrae in the disc space) is also performed. This may be performed using minimally invasive techniques. The fusion keeps the spine in its newly realigned position.
What Conditions are Treated with Spinal Reconstruction?
Spinal deformity reconstruction is used to treat a wide variety of conditions that result in the spine being misshapen; these include scoliosis, kyphosis, Scheuermann’s disease and others.
While there are many different ways to reconstruct the spine, the exact surgery for spinal deformity performed will depend primarily on the location and severity of the curve(s). Described below are general descriptions for anterior interbody fusion (ALIF) and posterior lumbar fusion (PLF) with pedicle screws. If a large number of levels of the spine are involved, the front and back side surgeries may be done on separate daysThere are many things you can do to positively affect the outcome of your surgery. These include:
Smoking cessation (nicotine abuse increases risk of complications, including fusion failure)
Ensuring good nutrition (specifically, adequate protein and calories to heal your wound), take supplemental protein shakes after surgery if you have any trouble getting enough with a regular diet
Vitamin D supplementation (1,000 units per day before and after your surgery to make sure you are not deficient)
Know your bone density (a bone density test can be done before surgery, if you have risk factors for osteoporosis)
Have an accurate list of your medications and how you take them
Get cleared by your primary care physician (and cardiologist, if you have one) for surgery to help avoid last minute discoveries of unresolved medical issues
Discuss how to handle your medications around the time of surgery with your surgeon and the doctor who prescribes them to make sure everyone is on the same page, for spine fusion surgery you will generally need to temporarily hold blood thinning medications/aspirin and anti-inflammatories, as well as certain other medications which should be determined by your treating doctors
Make sure any other significant medical issues are resolved/stable before you proceed (some issues may result in a last minute cancellation of your surgery if they are significant enough to affect the safety of the procedure)
Improve your fitness level if at all possible. Increasing your level of activity even for a few short weeks can be helpful in improving your heart and lungs for surgery and recover. You will also likely have an easier time mobilizing with physical therapy.
Avoid increasing your pain medicine usage, and try to reduce it if possible. Your body develops tolerance to pain medications the more you are exposed to them, which means that over time and repeated usage their effect becomes less and less.
Robotic spine Surgery
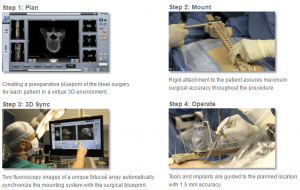
At Abhinav Gupta offers the most advanced Robotic Spine Surgery in the world. As Robots have invaded the field medicine with new age technology, which include analytical tools, multiple-source data, precision guidance, optical tracking, intra-op verification and connectivity.
He is the best spine surgeon in Delhi for robotic Spine surgery in selected cases. He offers the best minimally invasive spine surgery in Delhi NCR.In study presented the complication rates for the pedicle screw placement are :
• Robotic guidance: 4 percent
• Fluoroscopic guidance: 5.4 percent
• Freehand: 12.8 percent”. This analysis demonstrated that use of robotic guidance MIS can significantly reduce surgical complications and revision surgeries when compared to fluoro-guided MIS in the hands of experienced MIS surgeons.
Dr Abhinav Gupta has worked extensively on Brain Suite with MRI guided surgery. He has extensively studied robotic guidance and preplanning with brain surgery. Based on a preoperative plan, the robot drives the arm along planned trajectories, allowing the surgeon to implement the planned intervention. ROSA Spine ( Robot), involves a similar platform to the brain robot, but is able to adjust for patient movement during surgery. The researchers found the robot-assisted insertions demonstrated biomechanical superiority in terms of “alleviation of stress increments at adjacent segments” following fusion.
A new study published in Clinical Spine Surgery examines patients who underwent spinal deformity correction with robotic guidance for S2-alar-iliac screw insertion. The average screw length was 80 mm and all 31 trajectories were confirmed as accurate. None of the screws were intrapelvic or risked visceral or neuromuscular structures, and none of the screws required removal or revision.
Mazor Robotics Renaissance™ is transforming spine surgery from freehand procedures to highly-accurate, state-of-the-art procedures that may reduce fluoroscopy—even for minimally-invasive surgery (MIS), scoliosis, and other complex spinal deformity cases.
Powered by Clinically Validated Technology — Highly Accurate and Safe.
- 1.5 mm accuracy
Wide Range of Clinical Applications
Hardware and software tools enable a variety of spine procedures
- Open, MIS, and Percutaneous posterior thoracolumbar approaches
- Scoliosis and other complex spinal deformities
- Pedicle screws – short and long fusions
- Transfacet screws and translaminar-facet screw.
- Osteotomies
- Biopsy
Dr Abhinav Gupta offers the best back pain treatments in the country with his dedicated team. We offer full range of treatment with world renowned spine team for the Back pain and Neck pain treatments. We are the best spine centre in Delhi, Best spine centre in Noida, best spine centre in Ghaziabad. We offer full range of services for spine treatments, getting our patients back to life without requiring surgery .Infact nine out of ten patients recover with non surgical back pain treatments. Dr Abhinav Gupta’s “surgery as a last option” approach to treat back pain has been corner stone of his philosophy for more than 20 years.
Below is the list of treatments in which we specialize. The spine specialists here are leaders in surgical treatment options from the most common outpatient procedure to most complex cases.
CERVICAL SPINE SURGERY
Laminectomy decompression
Anterior cervical Discectomy
Endoscopic Discectomy
Posterior Cervical fusion with lateral mass screws
Anterior Cervical Discectomy and fusion
Dynamic stablisation/ Cervical disc replacement
Minimally Invasive spine surgery/Endoscopic spine
Spinal Tumors
Percutaneous spinal surgery
C-V Junction
Treatment of CVJ instability is challenging field in neurosurgery and is pri-mary indication for OC fusion. The common result is cervicomedullary neural tissue compression with development of symptoms and signs. Patients may present with progressive myelopathy, pain (neck pain, radiculopathy), lower cranial nerve dysfunction, or deformities of the craniocervical region. We reviewed 12-year experience of clinical outcome, occipitocervical instrumentation and operative morbidity in treatment of CVJ instability and lessons we learned are discussed.
Decision making
The indication for fusion in CVJ instability patients, an extensive posterior instrumentation fixation procedure that sacrifices the motion of the occipital and C1-2 complex is still controversial. In other words, failed fusions were due to use of an inappropriate method of rigid internal fixation or of an improper fusion level. To determine the number of fusion level is one of the most important factors to achieve the complete fusion. Reducibility, status of posterior element and direction of surgical approach should be determined in deciding the level.
We propose an algorithm for treatment of patients with CVJ disease (Fig. 5). An initial distinction should be made between non-trauma versus traumatic lesion and reducible versus irreducible lesion. We should always take the followings into consideration for specific treatment of CVJ instability.
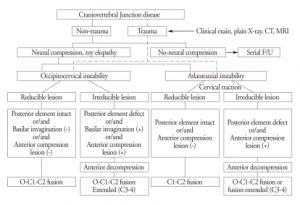
Algorithm for treatment of craniovertebral junction disease.
First is reducibility of the bony lesion. Depending on the reducibility and status of posterior element, the instrumentation is extended upward to the occiput or is extended downward to the C3, C4 fusion Incomplete reduction of C1-2 lesion is a statistically significant risk factor for VA injury during the placement of screws instrumentation. In reducible lesions at CVJ, stabilization is paramount to maintain neural decompression. In irreducible lesions, decompression is mandated at the site of encroachment, whether this is anterior or posterior approach. If complete reduction of the C1-2 subluxation is possible, we usually perform C1-2 fusion so that occipital-C1 motion is preserved. If the lesion is irreducible C1-2 subluxation and C1 or C2 posterior element defect (such as fracture and tumor), we recommend OC fusion in this circumstances. However, irreducible C1-2 lesion may necessitate OC fusion for stability.
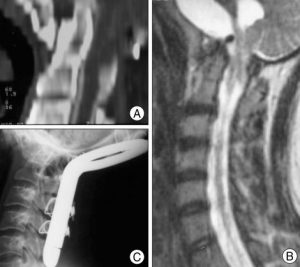
A 25-year-old female patient who had 7-years history of unsteady gait. A : Sagittal reconstructed CT scan shows the existence of basilar invagination. B : Preoperative MRI scan shows ventral compression of the cervicomedullary junction, associated Chiari-malformation. C : Lateral radiograph shows occiput to C3 fusion with foramen magnum decompression and C1 laminectomy. Postoperatively, she made a good recovery with resolution of her symptoms at last follow-up.
Second is direction of compression and encroachment. Compressed lesions require decompression at a site where the compression has occurred; these are divided into ventral and dorsal compression states. Anterior decompression (ex, transoral odontoidectomy) results in severe ligamentous and osseous destruction. This procedure alters CVJ anatomy and affects biomechanics of the region. The resultant occiput-C1 and C1-2 hypermobility requires OC fixation.
Third is the cause of the CVJ instability such as trauma or non-trauma, including congenital, inflammatory and tumor. CVJ instability represents the primary indication of CVJ fusion. Traumatic CVJ instability is often encountered in neurosurgical field and the neurological consequences are usually serious and fatal. However, once CVJ instability is confirmed in trauma patients, there should be no limitation in surgery to stabilize CVJ lesion regardless of abscence of neural compression. In cases of non-trauma, it is difficult to decide surgical treatment in children with craniovertebral junction diseases such as Grisel’s syndrome, osteogenesis imperfect and allied conditions. If there are no neural compression and osseous instability, re-evaluation with diagnostic procedures aimed at identifying the status of the bony development and neural compromise should be carried out on a yearly basis.
Our experience has shown that this algorithm regarding management of CVJ disease should be followed carefully to avoid unnecessary procedures but nevertheless, it is more important to provide surgical treatment based on different individuals.
Clinical outcomes
The effectiveness of operative procedures reported was demonstrated by the fact that each patient was either stabilized or improved at last follow up. Although there is no standardized grading system to clinically evaluate patients with cervical myelopathy, studies usually employ myelopathy grading system such as the JOA score and the Nurick Scale. In our series, 18 patients (78.3% of patients) experienced an improvement of the JOA scores in their symptoms after the operation. These results are consistent with the 75% to 95% rate reported in the literature.
Significant neurologic improvement (recovery rate > 50%) demonstrated 40% of patients in rheumatoid arthritis, 50% in trauma and 40% in congenital anomaly. These results are consistent with other reports indicating a 30% to 40% significant improvement in myelopathy. Although, it is difficult to make a statistically firm conclusion due to the small sample size, recovery rate in myelopathy seems not to be affected by the fusion methods. Traumatic atlanto-occipital dislocation with survival is rare, as the neurological consequences are usually immediately fatal. In this series, one patient had an occipitocervical dislocation with a quadriplegia and died at 2 month after the operation. Patient had been bedridden for 2 months after surgery. The patient died of pneumonia and sepsis. Non-union associated with pseudoarthrosis occurred in two patients. One patient had a rheumatoid arthritis with C1-C2-C3 subluxation and the other patient had a traumatic C1-C2-C3 dislocation with osteoporosis (T-score : -3.2). In CT scan, there were non-union in bone fusion site probably as a consequence of poor bone quality (osteopenic bone) and slight C1-2 subluxation on dynamic radiographs without neurological impairment. Although pseudarthrosis was observed, two patients were old age (over 65 years old) and had no neurologic symptoms. Thus, we did not perform revision surgery for these 2 patients. We are following these case further, and we will consider fusion surgery if further instrumentation failure and/or neurologic symptoms appear.
Fusion rate
Many investigators have discussed postoperative fusion rates in CVJ patients in whom occipitocervical or atlantoaxial arthrodesis has been performed. Fusion rate of the CVJ lesion is remarkably successful as their reported fusion rates are 75% to 100%. Surgeons used structural bone graft with sublaminar wires with good results. Fusion rates with internal rod and sublaminar wires were 90% to 100%. Grob et al.reported the use of plates and either transarticular screws or subaxial lateral mass screws in occipitocervical fusions with excellent results. Fusion rates with the screw and plate constructs are 90% to 100%. Indeed, all studies have demonstrated very consistent high fusion rates with cervicovertebral junction fixation regardless of fusion met-hods and underlying pathology. In this present study, our overall fusion rate of 93% is similar to that reported in other series involving this procedure. Non-union associated with pseudoarthrosis occurred in two patients. One patient had a rheumatoid arthritis and the other patient had a trauma patient with osteoporosis. Although, this study’s numbers are too small to make a firm conclusion, but we have deduced from our experience in failed fusion cases that sometimes wiring may appear superior to screws in patients with profoundly poor bone condition (e.g., rheumatoid arthritis, osteoporosis) which provide poor support for metal implants. We didn’t compare fusion rates according to the wire-rod/screw based construct, disease group or fusion methods separately, because we didn’t assess the fusion status of all patients with CT scan but assumed the success of fusion with dynamic X-ray in some patients. Also, this study is limited by study design (retrospective study), variability in patient selection and follow-up, as well as differences in surgical techniques over follow up period.
Wiring or screwing
The highly specialized anatomy of CVJ region have contributed in the development of fusion techniques for stabilization. Fusion procedures at the CVJ region must be capable of withstanding the forces of compression, axial loading, flexion, extension and rotation. Early techniques used standalone onlay bone grafting with the use of wires to secure bone grafts. It was not fully sufficient to stabilize until full arthrodesis and was needed to use postoperative halo fixation. Semi-rigid fixation using rod-and-wire techniques with bone grafting was developed and provided immediate stability and demonstrable higher fusion rate compared to previous techniques25).
Wiring constructs remain as an excellent method for stabilizing the craniovertebral junction and upper cervical spine. When wired to spine and skull, bone struts or metal implants provide reasonably good mechanical stabilization properties with a low incidence of complications. Sonntag and Dickman described the wire-rod technique; they used a grooved titanium fixation rod which was bent into a “U” shape and contoured to fit the cervical curvature . Rod and wire techniques are associated with lower rates of arthrodesis than rigid screw/rod systems probably due to biomechanical differences. Rod and wire techniques often require postoperative halo immobilization and fusion of additional mobile segments for adequate strength, and are associated with complications arising from the passage of sublaminar or suboccipital wires, including dural lacerations and neurological injuries. Major advantages of rod-and-wire techniques are greater ease of application and decreased risk to neurovascular structures. C1-C2 rod and wire technique is an excellent treatment option in patients with anatomical constraints that limit C1-C2 screw fixation and in young patients with immature spines. Continued development led to the creation of biomechanically superior segmental screw-based constructs for CVJ fusions.
Screw-based construct is technically demanding and requires operative precision and expertise when placing screws in the cervical vertebrae. Early screw-based constructs consisted of screw and lateral mass plates. These constructs provided increased stability and better outcomes when compared with prior instrumentation. The latest generation of fixation devices are polyaxial screw and rods, which can easily be bent in virtue of varying screw trajectories and apply the appropriate occipitocervical angle. Recent biomechanical studies have shown that the screw-based construct is more rigid than the wire-rod construct and reduced the need for external orthoses, but it is rather unclear whether it will result in higher rate of fusion. Reports of fusion rate of 80% after wiring and of 94% after screwing do not appear to influence markedly in final clinical results. Complete fusion can be achieved by increased number of wired vertebrae and by external immobilization in wire-rod system.
Complication
Potential intraoperative complications include excessive venous hemorrhage, neural tissue injury, VA injury, and dural lacerations. Most venous bleeding occur during the exposure of C1 lateral mass or C2 pars interarticularis which can be prevented by maintaining a subperiosteal plane of dissection. Hemostatic agents such as thrombin-soaked Gelfoam, or powdered Gelfoam can be used if necessary. One of the most troubling complications is damage to one or both vertebral arteries. Screw-based (plate or rod) construct has been shown to be an effective for treating atlantoaxial instability. However, despite the increased stability provided by the transarticular screw technique, there is the potential for VA damage and subsequent catastrophic neurological injury. A recent survey of neurosurgeons demonstrated a rate of known VA injury of 2.4% and a suspected injury rate of 1.7% per patient treated. One of the most common anatomical variants that places a patient at greater risk of VA injury is a high-riding transverse C-2 foramen. In other technique of atlantoaxial fixation, lateral mass screws are placed in the atlas which is connected via a rod or plate to the C-2 pedicle or pars interarticularis screws. Many believe that the risk of VA injury is less with this technique compared with transarticular screw placement. Because an axial screw travels just medial to the transverse foramen using this technique, there is still the potential for VA injury. The potential for VA injury in which the C1-C2 screw fixation technique is used can be minimized with careful screening using preoperative computed tomographic angiogram. If VA injury occurs, the bleeding is initially controlled by placing a screw in the drill hole. Prompt angiographic evaluation is mandated postoperatively. If there is evidence of VA injury, and the injured artery is still partially patent, it should be occluded provided the contralateral vessel normal (Fig. 4). This avoids the later development of an arterial dissection or a pseudoaneurysm or arteriovenous fistula.
The dura may be lacerated during sublaminar passage of the occipital or cervical cables or when occipital burr holes are made. These should be primarily repaired or usually controlled by using glue over the burr hole. Delayed complications include wound infections, loss of reduction, and failure of fusion. The management of wound infection is similar to that of any other postoperative spinal infection. Failure of arthrodesis necessitates surgical re-exploration if there is persistent bony instability.
Lesson we learned
We believe that success of the CVJ fusion depends on avoiding neurovascular structure, especially VA, injury during C1-2 screw placements. Although, number of cases was small and flow up period was short, we have kept key points in mind to improve patient safety, and outcomes and operative efficiency.
First is the patient’s positioning. Positioning in disease entity does not differ significantly. However, to keep the patient’s position neutrally is important in placing the screw. Surgeons can check the lateral screw trajectory intraoperatively by using fluoroscopy. But, it is difficult to identify patient’s midline and to check the screw position using fluoroscopy on anteroposterior view because the patient is placed in radio-opaque head fixation (ex, Mayfield three-point fixation). If patient’s position isslightly tilted left or right side, accurate screw placement maybe difficult increas-ing the risk of neurovascular structure injury.
Second is the preoperative planning in detail. Nowadays, 3D-reformatted CT scan provides substantial information of anatomical features of C1/ C2 and pathway of the vertebral artery. Before surgery, we should obtain a clear understanding of the anatomical landmarks essential in determining the starting point for screw trajectory. The screw starting point is measured in millimeters from the mid portion of the C1/C2. The screw trajectory is defined in number of degrees from both the parasagittal plane and the dorsal or ventral position of the screw relative to the VA foramen.
Third is placing the first screw on the most easily approachable and safest side. As a general rule, we start on the “best side” for screw placement so that at least one good screw is inserted as part of the construct. Conversely, if placement with the screw on the more difficult side is attempted first and results in a VA injury, placement of a second screw should not be attempted. This failure to place both screws might result in reduced stability and require postsurgical immobilization.
CONCLUSION
The clinical outcomes of our series show that the occipitocervical fusion with screw and wire system is a safe and effective method for the treatment of CVJ instability. Some may consider that wire-rod construct is “old fashioned”, but it still has a major role in spinal surgery. The advantages of the wire-rod device include being technically simple, safe and economical. The screw-rod device offers several advantages, including strong occipital screw purchase, easy contour of the rod to fit the occipitocervical curvature and allowing cervical decompressive procedures. There is no “best” method for occipitocervical fixation. We recommend that the spinal fixation technique should be individually selected based on the location and extent of the injury. Accurate imaging diagnosis and strict patient selection are keys to successful outcome.
Cervical Spine
Cervicl disc replacement
Defining Cervical Disc Replacement and Cervical Fusion
Cervical disc replacement involves removing the damaged disc, preparing the surfaces of the vertebrae, and installing a metal or plastic manufactured disc that, as mentioned, is shaped like a small hockey puck. With a cervical fusion, the damaged disc is also removed, but instead of replacing the disc, hardware is used to bolt the two (or more depending on how many levels are involved) vertebrae together. Within a few months, the vertebrae grow together, fusing into a solid mass of bone.
What sets cervical disc replacement apart from cervical fusion is that the disc replacement retains movement in the involved area of the neck while the fusion permanently and irreversibly disables movement. As a concept, disc replacement is supposed to be an alternative to fusion that will eliminate pain and won’t disrupt function, thereby lessening the risk of adjacent segment disease (ASD).
ASD is damage caused to the spinal segments both above and below the neck fusion, and this occurs when they become overloaded while trying to take on the extra forces the fused levels can no longer accomplish. Arthritis and bone spurs typically develop with ASD. As ASD advances, many patients will opt for more fusions in a desperate attempt to chase the damage and pain, but this will only make matters worse. Unfortunately, however, ASD doesn’t only occur following cervical fusion. Let me explain. To better understand ASD, see my video below:
Pain after Neck Fusion
Cervical Disc Replacement Side Effects and ASD
Cervical disc replacement certainly seems less extreme than a cervical fusion. It doesn’t eliminate movement. With the exception of the artificial disc device, no hardware (screws, rods, etc) is left attached to the spine. However, disc replacement is also a big surgery all on its own that’s associated with many side effects (e.g., metal ions in the blood due to wear and tear from the disc device, revision surgeries, chronic pain, etc.).
Last year I covered research that discovered another big problem in the list of cervical disc replacement side effects. Despite the push toward cervical disc replacement over cervical fusion due to fusion’s association with adjacent segment disease, ASD is also occurring is segments above and below disc replacements due to distorted movement in the spine. Why? Likely because an artificial disc simply can’t perfectly mimic the precise function of a normal biologic disc, so it’s understandable that abnormal motion in a segment of the spine is going to overwork adjoining segments that attempt to compensate.
Now, a new study seems to further support these findings on these specific cervical disc replacement side effects…
Cervical Disc Replacement Has the Same ASD Risk as Fusion
The new study was a meta-analysis, meaning many similar studies were aggregated to investigate like data, in this case the presence of ASD on radiology imaging following cervical disc replacement or fusion. After compiling all the data, researchers found no convincing evidence, based on radiology reports, that cervical disc replacement significantly decreased adjacent segment disease risk when compared to the fusion cases.
I can’t overstate the magnitude of this research finding! First, this is a meta-analysis that looked at data from many different studies, so this just isn’t just the finding of one study. Second, the main reason to get a disc replacement is that it’s motion preserving and that this is supposed to reduce the likelihood of ASD or eliminate it all together. In fact, if that’s true, I’m not sure why anyone would want a disc replacement.
The upshot? This meta-analysis should be the death knell for disc replacement. That’s because the only raison d’être for disc replacement was that it could reduce the ASD side effects compared to fusion. If it can’t do that, why would anyone want a disc replacement? Why is this still happening? A big neck surgery is a big neck surgery is a big neck surgery. They all end up destroying critical stabilizing structures in the neck.
