Dr. Abhinav Gupta
MBBS DNB (MCh Neurosurgery) FINR
Fellowship in Minimally Invasive Spine Surgery (Univ. of Chicago )
Fellowship in Interventional Neurosurgery (Univ of Zurich, Swiss)
Senior Consultant Neurosurgeon & Spine Surgeon
Senior Pain Specialist
Interventional Neurologist
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
What is Neuro-Ophthalmology?
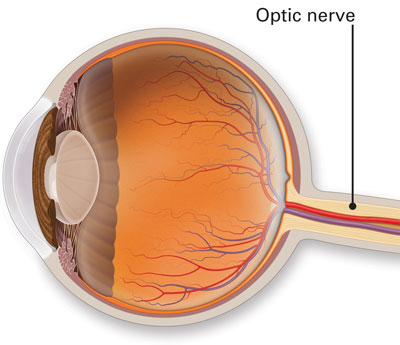
Neuro-ophthalmology is an ophthalmic subspecialty that addresses the relationship between the eye and the brain, specifically disorders of the optic nerve, orbit, and brain, associated with visual symptoms. Neuro-ophthalmologists provide comprehensive clinical care to a broad spectrum of patients with visual disturbance from optic nerve diseases, central nervous system disorders,
The Visual Evoked Potential (VEP)
VEP measures the electrical responses generated at visual cortex in response to a visual stimulus with the help of electrodes. It is helpful in: Optic nerve disease Cortical Blindness Visual assessment in preschool children Malingerers Amblyopia A special type of flash VEP is helpful in cases with media opacity as a rough
The Electro-oculogram (EOG)
This test examines the function of the retinal pigment epithelial cells (RPE). When this layer is healthy a standing potential is established between the front and the back of the eye that responds to change in background illumination. The standing potential can be measured by measuring the voltage induced across
The Electro-Retinogram (ERG)
The ERG is the mass electrical response of retina in response to a bright flash of light and is recorded using corneal electrodes. It reflects the function of the retinal photoreceptors (rods and cones) and the inner nuclear layers of retina. It is often useful for:- ” Diagnosing and predicting
For further information consult The Neuro-Ophthalmology Service at Neuro Spine and Pain
Ocular Electrophysiology (Electrodiagnostics) Electrophysiological examination provides objective information in relation to the function of the visual pathway helping in diagnosis and management of the patient. The main tests are Electro-retinogram (ERG), Visual evoked potential (VEP) and Electro-oculogram (EOG). These are used to locate the site of disease whether in the retina,
The steroids made my eyes much more comfortable. Can’t I just continue taking them?
Steroid therapy may be effective in halting the inflammatory phase of thyroid orbitopathy and partially shrinking the muscle swelling. Steroid side effects are very common with continued treatment. If there are still problems with eye movements (double vision), exposure problems (irritation and foreign body sensation), or decreased vision then surgery
What is the treatment for thyroid eye disease?
In patients with mild involvement, irritation and foreign body sensation may improve with artificial tears and the use of lubricating ointment at night. If the lids are not closing completely, they may be taped closed at night. With more severe corneal problems, lid surgery to help partially close the lids
What is the prognosis of thyroid eye disease?
Thyroid orbitopathy, like other autoimmune diseases, often comes and goes on its own. There is frequently only one acute inflammatory episode but unfortunately the effects may persist for years or even permanently. Although there may be some reduction of the prominence of the globe, eye movements will often not return
What tests are done to detect thyroid eye disease?
This is detected by carefully checking vision, pupillary reactivity, visual fields, and the appearance of the optic nerve head. Most frequently this makes the thyroid gland over produce thyroid hormone that in turn can lead to tremors, shakes, weight loss, rapid heart beat or palpitations, nervousness, and sensitivity to heat.
How will I know if I have thyroid Eye Disease?
With muscle enlargement the globe (eyeball) is pushed forward leading to the characteristic “stare.” In addition, the muscles become stiff and the upper lid tends to retract, pulling away from the colored portion of the eye. The eyes may become red due to difficulty closing as well as increased prominence
What is Thyroid Eye Disease?
This is an autoimmune condition where your body’s immune system is producing factors that stimulate enlargement of the muscles that move the eye. This can result in bulging of the eyes, retraction of the lids, double vision, decreased vision, and ocular irritation. This is often associated with abnormalities in thyroid
How is papilledema treated?
Reduction in CSF production or increase in its outflow may reduce intracranial pressure. Weight reduction programs (in overweight patients) may be effective. Continuous drainage may be surgically accomplished by placing a catheter between the spinal canal and the abdomen (lumbo-peritoneal shunt). In patients with worsening visual fields or decrease
How is the cause for papilledema detected?
The patient requires a MRI scan. The diagnosis also requires a spinal tap. This will document elevated pressure inside your head and make sure there are no other abnormalities in the CSF. The finding of abnormal cells, inflammatory cells, or elevated protein may indicate a previous infectious, inflammatory, or tumor
How will I know if I have papilledema?
The most common symptoms of high intracranial pressure are headache and visual loss. The headache may be located anywhere; frequently in the back of the neck. It is usually steady but may be pounding. It may be very severe, and unlike migraine, it may awaken the patient in the middle
What is papilledema?
This is a condition in which high pressure inside your head can cause problems with vision and headache. In papilledema cerebrospinal fluid outflow is blocked. The pressure is transmitted to the back of the eye via the optic nerve sheath (surrounding each of the optic nerves) producing the swelling seen
Will my vision get better?
In patients with visual loss due to compression of the optic nerve or chiasm by a pituitary tumor the chance of visual improvement is best predicted by the duration of the damage. The presence of changes in the back of the eye (optic atrophy) may suggest long duration. Surgery also
How is a pituitary tumor treated?
When the patient is symptomatic, some form of treatment is usually indicated. The most common approach is surgery usually performed through the nose (or up under the lip). Occasionally (especially when the tumor is larger or extending to the side) a surgical approach may be best through a scalp incision.
How is a pituitary tumor detected?
Pituitary tumors are usually suspected based on endocrine changes but are confirmed with imaging studies. A CT scan can reveal a pituitary tumor and may be especially sensitive to hemorrhage. MRI scanning may be more sensitive and better define the relationship of the tumor to the optic nerves and surrounding
How would I know if I have a Pituitary tumor?
Patients with pituitary tumors often have no symptoms at all. Occasionally these tumors may produce headaches. Head pain may be sudden and severe if there is a bleed into the tumor. Endocrine symptoms are most common including alterations in menstruation, lactation (milk from the breast), impotence, or loss of sex
What is a Pituitary Tumor?
Pituitary tumors are benign (non-cancerous) overgrowth of cells that make up the pituitary gland (the master gland that regulates other glands in the body). Tumors that grow large enough to produce symptoms are less common but still are one of the most common tumors occurring within the head.
Do I have Multiple Sclerosis (MS)?
Multiple sclerosis (MS) is a disease process where the body’s immune system attacks multiple areas in multiple episodes. An episode of optic neuritis may be the first indication of multiple sclerosis. With a single episode, without other evidence of involvement, we usually cannot make the diagnosis at that time.
How is optic neuritis treated?
Patients treated with oral (pills) steroids seem to have a higher chance of recurrent episodes. Therefore, steroid pills alone are not recommended as treatment. Patients who were treated with intravenous (given by needle) steroids did have a slightly more rapid recovery of their vision, although the final visual outcome
What will happen to the vision over time?
The pain will go away, usually in a few days. The vision problems will improve in the majority (92%) of patients. There are rare patients who have continued progressive loss of vision. Frequently colors look different or “washed out.” Visual recovery usually takes place over a period of weeks
How does the ophthalmologist know that I have optic neuritis?
A few patients with optic neuritis have swelling of the optic disc (the beginning of the optic nerve) at the back of the eye. This is referred to as papillitis. One sign usually detected by your eye doctor is the presence of an afferent pupillary defect.
What are the symptoms of optic neuritis?
The most common symptom of optic neuritis is sudden decrease in vision. In mild cases, it may look like “the contrast is turned down” or that colors appear “washed out.” This may vary and, not infrequently, will progress from the time it is first noticed. The second most common symptom
What is Optic Neuritis?
This is the most common cause of sudden visual loss in a young patient. It is often associated with discomfort in or around the eye, particularly with eye movement. The optic nerve fibers are coated with myelin to help them conduct the electrical signals back to your brain.
What do I do about the double vision?
Since we expect the double vision to clear up on its own any treatment will hopefully be necessary for only a few weeks or months. The easiest way to get rid of the double vision is to wear a patch. Alternatively one lens of your glasses may be fogged
What is the outcome of nerve palsies?
There is no known means of accelerating the natural recovery characteristic of microvascular cranial nerve palsy. It is important to make sure that blood pressure and blood sugar are adequately controlled. The double vision may be treated acutely with patching either eye.
What tests are done for nerve palsies?
While it is possible for multiple cranial nerve palsies to have a microvascular cause all patients with more than a single nerve palsy or with other neurologic findings must have a work up (neurologic examination and imaging study) before the diagnosis is accepted.
How do I know that I have cranial nerve palsy?
Dysfunction of one cranial nerve will produce weakness in one or more muscles. If the eyes aren’t moving together the patient will experience blurred or double vision. If only the VIth nerve (innervating the lateral rectus) is affected the double vision will be side to side.
What is Cranial Nerve Palsy?
This is one of the most common causes of acute double vision in the older population. It occurs more often in patients with diabetes and high blood pressure. These will get better and essentially always resolve without leaving any double vision. However, compressive masses, infections, inflammation and injury can also
What is the treatment for AION?
Unfortunately, at this time there is no proven treatment for patients with AION. It has been suggested that aspirin (regular size or baby aspirin once a day) may decrease the chance of an episode in the opposite eye. It is important that the blood pressure be followed by your doctor
Will I get back my vision?
Most patients with ischemic optic neuropathy will have relatively stable vision. A recent study suggests that 40% of patients may expect to have some improvement in central vision. A very small number of patients can have worsening of vision.
What are the symptoms and tests for AION?
Most patients with AION notice a sudden painless disturbance in their vision. Because of the decreased optic nerve function, however, the pupils may not react as well when light is directed into the affected eye. Swinging a flashlight between the two eyes will then show an “afferent pupillary defect.”
What is Ischemic Optic Neuropathy (AION)?
This is the most common cause of sudden decreased vision in patients older than 40 years. We do not see with our eyes. We see with part of our brain that is capable of interpreting visual signals sent back from the eyes.
What are the common types of neuro-ophthalmic diseases?
A few of the most common neuro-ophthalmic conditions are optic neuritis, ischemic optic neuropathy, compressive optic neuropathy (including pituitary tumors), papilledema, inflammatory and infectious optic neuropathies, cerebrovascular disorder involving vision, tumors involving vision, blephrospasm & hemifacial spasm, thyroid eye disease, myasthenia gravis, ocular motor disorders (including cranial nerve palsies), pupillary
What are the common symptoms of neuro-ophthalmic diseases?
Symptoms that are more common in neuro-ophthalmic disease include visual loss, visual disturbance, diplopia, unequal pupils and eyelid and facial spasms.
