
Neuro Intervention
These are minimally invasive procedures for brain and spine, done in a Neuro-cath lab (Neuro Intervention Suite)
Neuro Intervention
Dr Abhinav Gupta is the Best Interventional Neuroradiologist in Delhi, NCR. He has had extensive training in both India and abroad and mastered these techniques. He offers Endovascular (Neuro-surgical treatment via blood vessels) for lesions of the head, neck, spine, brain, and spinal cord.
Neurointervention:
These are minimally invasive procedures for brain and spine, done in a Neuro-cath lab (Neuro Intervention Suite). The surgeon inserts a catheter resembling long tube into the groin and thread it up through the vessels at the problem site. Once the catheter is in place depending on the condition the surgeon can deliver medications or utilize the medical device to accomplish treatment.
For spinal anomalies resulting from a compression fracture, tumor of the spine or narrowing of the spinal canal, the surgeon will insert cannula’s resembling like a tube, directly to the problem site and work through them to lessen any pressure on the nerve region in order to relieve the patients of pain.
In both the cases, the surgeon uses the minimally invasive technique which also transmits internal images of the brain or the spine on a large screen where the procedure is carried out throughout the procedure allowing them to clearly visualize the problem area.
There are best possible treatment outcomes even when the neurointerventional treatment is considered as less invasive than other traditional methods hence are more attractive options to patients.
There are many conditions of brain and spine which can be treated with neurointerventional procedures, some of them are:
- Aneurysms
- Strokes
- Spinal compression fractures
Although this technique is not fit for all treatment for every individual patient case that falls within this category, these surgical technique has proven benefits over traditional treatments, benefits like:
- Shorter recovery time
- Fewer complications
- Less post-operative pain
Endovascular therapies available:
- STROKE treatment
- Aneurysm Coiling
- AVM Embolisation
- Tumor Embolisation
Nonvascular Interventions include:
- Pain Management
- Percutaneous Biopsies
- Percutaneous Vertebral Augmentation
- Percutaneous Management of Disk disease
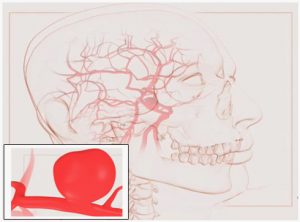
Brain Aneurysm is a weak and dilated area of a blood vessel in the brain. As the wall is weak they tend to rupture if there is increase in BP leading to bleeding in brain known as Subarachnoid Hemorrhage (SAH). They can also cause stroke or permanent nerve damage. The Aneurysms vary in size, shape and location .and are generally diagnosed after rupture.
Diagnosis
It is by doing a Cerebral angiogram for which Digital Subtraction Angiography is taken as gold standard . A Cerebral angiogram can detect the degree of narrowing or obstruction of an artery or blood vessel in the brain, head, or neck, and can identify changes in an artery or vein such as a weak spot like an aneurysm or an AVM.
Treatment
Surgical clipping: Where a clip is applied to the neck of the aneurysm to remove it from the circulation thus preventing any further bleed. It is considered traumatic but curative.
Coiling of the aneurysm: In this procedure the aneurysm is entered via catheter and small coils are deposited in the aneurysm to fill it. These coil promote thrombosis within the aneurysm and significantly decreases the chances of re rupture
Tumor embolisation: Here as we can see
- MRI of a large meningioma.
- External carotid angiogram before embolisation.
- Selective angio of the feeder ie Middle Meningeal
- Photomicrograph of Bead micro emboli.
- Image after embolisation with PVA particles.
The tumor was later resected with minimal blood loss.
.,
Detachable silicone balloons uninflated (A) and inflated (B). Carotid-cavernous sinus fistula before embolization (C) and after embolization (D) with Gold Valve detachable balloons.
View Media Gallery
Of the endovascular therapies, embolization of aneurysms (see the image below) is one of the principal procedures. Although all patients with ruptured or unruptured aneurysms should be evaluated for endovascular therapy, not all patients are best served with this therapy. Conventional surgical clipping is still a consideration. In selecting appropriate therapy, the referring and interventional physicians should consider the configuration of the aneurysm and its neck, the location and number of the aneurysms, and the patient’s preference and overall physical condition (eg, ability to tolerate anesthesia and surgery). The risks and benefits of each therapy should be evaluated on a case-by-case basis. The conclusions and recommendations should then be presented to those patients who are able to give consent, their families, and the referring physician.
Large ruptured aneurysm before embolization (A) and after embolization (B, C) embolization with Guglielmi detachable coils.
View Media Gallery
Embolotherapy
Although the practice of embolotherapy has existed for approximately 40 years, active consideration of this therapy continues to evolve for the definitive or preoperative adjunctive management of aneurysms, vascular malformations, and vascular tumors. The progressive improvement in outcomes of endovascular therapy is principally the result of ongoing development and refinement of microcatheter delivery systems and of safer and more varied embolic agents and devices. New microcatheters increase superselectivity, which in turn improves target-specific embolization with increased preservation of adjacent normal vascular anatomy. These microcatheters can be used to deliver all currently available embolic agents, including particulate emboli, coils, balloons, tissue adhesives, nonadhesive agents, sclerosing agents, and chemotherapeutic agents. [9, 10]
Particulate embolic agents
Particulate agents are the embolic materials of choice for occluding the microvascular supply of tumors and many hemorrhagic conditions. These agents are divided into 2 general categories: absorbable and nonabsorbable agents.
Absorbable agents
Absorbable agents, as their name implies, do not permanently occlude vessels and therefore are of benefit within the first few hours of therapy. Absorbable agents are most effective in the management of transient bleeding such as that associated with epistaxis or for preoperative devascularization of vascular lesions such as meningiomas and some hypervascular metastases. Materials in this category include gelatin sponge (Gelfoam), available as a powder of 40-60 µm in particulate diameter or in sheets that can be cut into large particle sizes or into pledgets. Microfibrillar collagen (Avitene) is supplied as a powder with a particle size of approximately 50 µm. It is widely used as a topical thrombotic agent in conventional surgery and provides a very rapid thrombosis of vessels treated endovascularly.
On occasion, absorbable embolic agents can be used to protect normal vessels. This technique temporarily occludes a normal vessel, allowing the redirection of flow of permanent embolic agents into the abnormal vessels. An autologous blood clot may be used for temporary, protective occlusion because it rapidly recanalizes. Likewise, a pledget of gelatin sponge can be placed in the origin of a normal arterial branch to ensure that the permanent embolic materials or chemotherapeutic agents infused proximally do not enter that vessel and that they are directed to the abnormal vessels.
Vessels occluded with autologous clot and/or Gelfoam pledgets recanalize in a short time, reestablishing flow to its normal territory. Abnormal vessels embolized with nonabsorbable agents, however, remain occluded, while those treated with chemotherapeutic agents remain open for repeat therapy. For large vessels of the cervical arterial anatomy, a similar utility is accomplished with the use of nondetachable, low-pressure balloon catheters. This technique is particularly effective when used to direct the flow of chemotherapeutic agents into vessels of the head and neck that are too small to be selectively catheterized while temporarily diverting flow away from normal vessels.
Absorbable agents are effective when used as preoperative adjunctive therapy immediately preceding surgery. However, the author’s philosophy is that preoperative embolization should be as complete and permanent as possible. The recommended approach requires the use of nonabsorbable agents, given the possibility of delayed surgery or incomplete surgical resection of the lesion. In the event of the latter, permanent embolization of the unresected portion of the tumor may improve the overall outcome. The use of permanent agents at the outset may obviate the need for repeat embolizations.
Nonabsorbable agents
The nonabsorbable particulate agents most commonly used are polyvinyl alcohol (PVA) particles. Prepackaged PVA particles are provided in a range of sizes, varying from one manufacturer to another. Particle sizes are typically 150-1000 μm in particulate diameter. The small particle sizes are most frequently used to embolize vascular tumors, whereas the larger sizes are most useful in occluding large, low-flow vascular malformations. In larger, higher-flow vascular pathology, macroembolic agents, including microcoils and occasionally suture material, can be used to build a framework or mesh against which microparticulate agents may accumulate (see the image below).
Arteriovenous malformation before embolization (A) and after embolization (B and C) with polyvinyl alcohol (PVA) particles, ethanol, and coils.
Vessels are embolized with PVA alone tend to recanalize after a few weeks. Although the particle itself is nonabsorbable, the extremely irregular surface of each particle creates a high coefficient of friction, which often results in adhesion of the particles proximally to the wall of the vessel without complete occlusion of the nidus. Blood flow is usually eliminated initially. However, the thrombus that forms between the particles may eventually recanalize. Neoendothelium covers particles remaining on the surface. This limitation is partially overcome by packing the vessel with high concentrations of small PVA particles followed by proximal occlusion with large particles or microcoils.
Different combinations of agents may be used to achieve a more permanent occlusion. Absolute ethanol mixed with particles will not only occlude the target vessel but also denature the vascular endothelium, resulting in a fibrotic reaction within the lumen and around the particles. Of concern, however, because ethanol is a nonparticulate and is extremely cytotoxic, is that ethanol is likely to pass through vessels with a diameter approximating the size of the particles, resulting in necrosis of perilesional normal tissue. In addition, alcohol in the external carotid system tends to be painful. Sodium tetradecyl sulfate injection (Sotradecol; Latham, NY) has been used as an alternative sclerosing agent because it does not produce as much pain as ethanol does.
Another alternative combination is a mixture of PVA particles and microfibrillar collagen. This combination offers a number of advantages. When mixed in contrast material, microfibrillar collagen forms a colloidal suspension in which the PVA particles remain suspended and somewhat evenly dispersed. This suspension, in turn, facilitates delivery of the particles through the small lumen of the microcatheter, decreasing the likelihood of impacting particles in the catheter and occluding it. This advantage helps to avoid a time-consuming exchange of catheters.
With an average particle size of 50 μm, microfibrillar collagen fills the gaps between the PVA particles, helping provide a more complete occlusion. Histologic studies have shown that microfibrillar collagen in occluded vessels will form a collagen matrix that adheres to both the endothelium and the PVA particles. This combination offers an advantage over the PVA-ethanol mixture in that it produces less patient discomfort and that it is less likely to pass through small anastomoses and injure adjacent normal tissue. After the PVA–microfibrillar collagen admixture is infused, the residual lumen of the abnormal vessel at the catheter tip may be occluded by using a platinum microcoil to reduce arterial pulsations against the occlusive particles. This coiling appears to slow the rate of recanalization long enough for luminal fibrosis to occur.
Long-term studies on the evolution of vessels embolized with PVA, microfibrillar collagen, and coils have not been conducted; however, in the author’s experience, this combination has proven to be effective in the treatment of vascular tumors of the head and neck. Microfibrillar collagen is not routinely included in intracerebral and intraspinal embolizations to minimize inadvertent embolization of the normal cerebral or spinal microvasculature.
Soft, smooth, deformable particles (Embospheres, Merit Medical; South Jordan, UT) and compressible microspheres of liquid PVA (Bead Block) tend to ovalize when confined, a trait that makes these agents effective in distal embolotherapy. Because they do not adhere to vascular walls as do crystalline PVA particles, these soft particles are most likely to reach the capillary bed of a tumor or nidus of a malformation. Both Embospheres and Bead Block can be tagged with chemotherapeutic agents and isotopes.
Coils
Historically, fibered, stainless steel Gianturco and Hilal coils were used to reduce or redirect blood flow in large arteriovenous malformations (AVMs), arteriovenous fistulae (AVFs), and hemorrhagic traumatic vascular injuries of the extracranial circulation. Magnetic resonance (MR)–compatible platinum coils have largely replaced MR-incompatible stainless steel coils. The older, larger coils are considerably larger in diameter than the microcatheter delivery systems currently used. Catheters 4F or larger are required with these 0.035-inch and 0.038-inch coils. Catheters of this size severely limit the distance into which a vessel can be cannulized. Unless the malformation is large, it is unlikely that coils of this size will reach the nidus.
The coil itself often does not produce complete thrombosis of the vessel, and it secondarily inhibits further embolization with other agents. Therefore, use of the large coils is limited to occlusions of large vessels in the neck and skull base, usually those occurring after penetrating trauma (see the image below). Proximal vessel embolization with larger coil sizes may help retard recanalization of distal vasculature embolized with smaller microcoils and/or particles.
A, Gunshot wound to the right side of the neck transects the right vertebral artery (RVA) and the right internal maxillary artery (RIMAX), with partial transection and pseudoaneurysm formation in the midcervical right internal carotid artery (RICA). B and C, Transected segments of the RVA and RIMAX are coil embolized. The RICA pseudoaneurysm was successfully treated with a 7 x 40-mm Wallgraft covered stent.
View Media Gallery
A variety of microcoils have been developed for use with the microcatheter systems to facilitate distal deployment in small vessels of the head, neck, and spine. Hilal coils, the earliest of the fibered microcoils, were effective but were relatively stiff and made of stainless steel. These were later replaced by a softer, platinum version that was MR compatible. Platinum microcoils 0.010 and 0.016 inches in diameter, with and without Dacron polyester fibers, are available for use with microcatheter systems and are supplied in a variety of shapes, sizes, and lengths. Most of these are woven with the small polyester fibers to increase their thrombogenicity. These small coils can be deployed just proximal to the nidus of a malformation if it is accessible with a microcatheter, or it can be directed by blood flow and floated peripherally if direct access to the nidus cannot be achieved. Microcoils are quite effective in the rapid establishment of hemostasis in traumatic vascular injuries.
The soft, Berenstein Liquid coils lack fibers and are intended to flow further into a vessel than the more rigid fibered coils. Because of the small size of these coils, distal occlusion is most effectively achieved. Flow velocity is often reduced to a point where subsequent particulate or liquid embolization provides a more thorough occlusion of the abnormal vessels. As previously mentioned, coils are also frequently deployed proximally in a vessel after particulate embolization to reduce the likelihood of recanalization. While one of the most useful devices in the armamentarium, it is unfortunate that they are no longer in production. No other similarly functioning coils are currently available.
Interventional management of aneurysms with detachable coils is distinctly different from management with nondetachable coils and is discussed separately in the following paragraphs.
Balloons
Detachable balloon macroemboli are no longer available. For the sake of completeness, a short discussion is included in this section.
The advantages of balloon embolization include the following:
- The ability to occlude a vessel at a precise location
- The ability to navigate attached, partially inflated balloons to distal locations along a tortuous course
- The ability to rapidly occlude vessels larger than the caliber of the catheter
- The ability to repeatedly inflate, deflate, and reposition the balloon until the desired position is achieved
The original latex balloons were manually bound to coaxial microcatheter assemblies with latex ligatures. Although effective, this technique was tedious and time consuming. Latex and silicone elastomer balloons with mitered valves were subsequently developed to facilitate attachment and detachment.
Latex and silicone balloons have different properties with respect to distensibility, time to deflation, and surface-friction characteristics. Latex balloons are more distensible and compliant than silicone balloons and therefore most readily conform to the shape of a vessel while reducing the risk of vascular rupture. Latex also has a far greater coefficient of surface friction than that of silicone balloons. This feature reduces the likelihood of balloon migration. These properties make latex balloons preferable for occluding large, high-flow vessels, as in trapping procedures, and for treating carotid-cavernous sinus fistulae.
In contrast, silicone balloons are relatively noncompliant and inflate to a preformed shape. Therefore, they are less likely than latex balloons to mold to the vascular contour. Because of their lowered coefficient of friction, they are more likely than latex balloons to migrate after detachment. Because silicone is less porous than latex, silicone balloons tend to remain inflated longer, averaging more than 24 weeks to deflation, versus 2-4 weeks to deflation for latex balloons.
While effective in their day, detachable balloons have largely been replaced with a wide variety of macrocoils and microcoils, which can be deployed more rapidly, through smaller delivery systems and at a lower cost to the patient.
Liquid embolic agents
Among the most notable liquid embolic agents are N -butyl cyanoacrylate (NBCA) and acrylic tissue adhesive. The acrylic tissue adhesive rapidly polymerizes on contact with any ionic substance, such as blood, saline, ionic contrast medium, and vascular epithelium. Polymerization time is prolonged with the mixture of various amounts of glacial acetic acid and/or oil-based contrast agents such as ethiodized oil (Ethiodol).
The flow velocity of an arteriovenous shunt may be reduced with other agents prior to NBCA infusion to minimize risk of the errant passage of glue into the venous system. For example, platinum microcoils may be deployed distally with the intent of reducing flow, not occluding flow, prolonging the length of time NBCA remains in the lumen of the target vessel for polymerization. The main advantage of this tissue adhesive is its ability to rapidly occlude high-flow AVMs, with a result that is more permanent than that possible with particulate agents. NBCA is more likely than particulate agents to reach and occlude the nidus of an AVM.
NBCA has a number of disadvantages. The catheter must be rapidly withdrawn after each injection of NBCA to prevent gluing the catheter tip to the vessel wall. This results in frequent, time-consuming catheter exchanges. If the lesion was difficult to access initially, considerable time may be required to reposition a new catheter into the vessel a second or third time if additional infusions are required.
Failure to rapidly withdraw the catheter increases the risk of gluing the catheter in place. Complications secondary to incorrect polymerization time add to the risk. Too short a polymerization time may result in proximal vessel occlusion and possible incorporation of the catheter tip. A prolonged polymerization time may result in passage of acrylic through the malformation and solidification in the venous outflow tract, increasing the risk of hemorrhage. Because the resultant glue cast is rigid, patient discomfort may be notable, and a foreign-body sensation may occur after embolization of lesions of the face, mouth, tongue, or neck. For these reasons, the use of NBCA is limited to the occlusion of high-flow AVMs of the brain and spinal canal.
The remarkable increase in demand for interventional procedures has spurred the development of embolic agents and devices that are safer and more permanent. Nonadhesive, flexible polymers offer all the advantages of NBCA without the risk of gluing a catheter in place or the need to exchange catheters after each infusion. One nonadhesive liquid embolic agent, Onyx, appears to be safer and more effective than NBCA in the treatment of high-flow AVMs. Onyx has the added advantage of forming soft pliable casts, which, unlike the more brittle NBCA, facilitates a less complicated surgical resection of embolized AVMs (see the image below).
Right temporal arteriovenous malformation (AVM) supplied by the right middle cerebral artery (RMCA) (A and B) and left vertebral artery (LVA) (C and D). E and F, Casts of nonadhesive liquid embolic agent (Onyx) in the feeders and nidus. G and H, Postembolization angiograms show no residual flow to the AVM.
View Media Gallery
Sclerosing agents
Absolute ethanol is the prototypic sclerosing agent. Solutions opacified with metrizamide powder have produced excellent results in the obliteration of large vascular malformations. Sodium tetradecyl sulfate (Sotradecol) behaves similarly to alcohol, but with less associated pain. As previously discussed, ethanol has been included in particulate admixtures, most notably with the admixture of microfibrillar collagen and PVA particles.
As a cytotoxic agent, ethanol facilitates tissue necrosis during tumor embolization. This effect is especially useful when treating neoplasms of nonneural origin. Risks associated with the use of ethanol include peritumoral swelling, pain, and necrosis of normal peritumoral tissue via normal microscopic anastomotic branches. Aggressive clinical monitoring during embolotherapy by an anesthesiologist is essential to reduce pain and to preserve an airway when lesions of the oropharynx and neck are treated.
In the author’s experience, embolotherapy with absolute ethanol, compared with the particulate agents alone and with NBCA, has resulted in a more permanent occlusion of abnormal vessels without the inherent risks associated with tissue adhesives.
Endovascular Management of Intracranial Aneurysms
History
The first descriptions of the endosaccular treatment of aneurysms were open surgical techniques, including magnetic direction of ferrous spherical emboli released in the proximal arterial anatomy and deployment of charged copper wires through an aneurysm dome. The work of Drs. Werner and Blakemore represented an extrapolation of the use of copper wire in the treatment of abdominal aortic aneurysms in the late 1930s. Although successful, these techniques did not offer outcome statistics better than that of conventional surgical clipping.
The initial endovascular management of aneurysms was based on the endosaccular deployment of appropriately sized latex balloons (see the image below) using an angiographic rather than an open surgical approach. Developed in Russia by Dr. Fedor Serbinenko in 1962, the technique was associated with a high incidence of aneurysmal rupture. This complication was believed to be the result of the rigid balloons having exerted asymmetric pressure on the walls of the aneurysms, resulting in a deformity of the aneurysm that frequently led to rupture.
While the use of endosaccular wires and balloons in aneurysm therapy was fraught with complications and short lived, these works inspired extensive research into the development of safer, more effective devices for the endovascular management of intracranial aneurysms. See the image below.
Detachable silicone balloons uninflated (A) and inflated (B). Carotid-cavernous sinus fistula before embolization (C) and after embolization (D) with Gold Valve detachable balloons.
View Media Gallery
Guglielmi detachable coil
Although the use of balloons to treat aneurysms quickly fell out of favor, Serbinenko’s work provided the momentum that eventually led to the development of a detachable-coil technique pioneered by Dr Guido Guglielmi in 1990. Numerous modifications of the Guglielmi detachable coil (GDC) have been made over the years, but the basic design remains the most widely used device for embolotherapy of intracranial aneurysms to date.
Endovascular management of aneurysms requires a coil with unique properties, including control and recoverability, softness, and maximum packability. GDC coils (Target Therapeutics, Boston Scientific, Stryker Neurovascular), are long, nonfibered platinum microcoils fused to a guidewire. These coils, the first to gain FDA approval, can be positioned, withdrawn, and repositioned repeatedly until the desired position is obtained. Detachment is then achieved by passing a low-voltage, low-amperage current through the guidewire to hydrolyze the connection between the guidewire and the coil. The current also initiates platelet and RBC aggregation, promoting thrombosis. These coils have a distinct advantage over detachable balloons in that the conformable platinum coils exert minimal and more uniformly distributed pressure on the wall of the aneurysm. This feature reduces the risk of periprocedural rupture, a problem inherent with the use of rigid coils and balloons.
Bioactive coils
A GDC variant called the Matrix coil (Target Therapeutics, Boston Scientific, Stryker Neurovascular) is coated with polyglycolic-polylactic acid (PGLA) copolymer that promotes fibrosis within and surrounding the coil mass, which is intended to improve the permanence of the procedure and promote shrinkage of the aneurysm. Alternatively, the Cerecyte coil (Micrus Endovascular, Codman Neurovascular) is a platinum coil with a bioactive PGLA copolymer core. Functionally similar to GDCs, they differ in that they are detached thermally rather than hydrolytically. Another device, the HydroCoil, is a helical platinum coil, coated with a hydrogel. The hydrogel expands in a fluid environment after deployment; however, the HydroCoil is not considered bioactive as hydrogel does not promote fibrosis as does PGLA.
Balloon-assist technique
Until the early 2000s, endovascular therapy could be offered only to patients with aneurysms of a configuration that were amenable to coiling; that is, the aneurysm had to have a relatively small neck that could hold the detached coils in place within the lumen of the aneurysm and out of the parent artery. However, with the he balloon-assist technique which uses extremely soft, compliant, nondetachable balloon catheters made of silicone. When inflated across the neck of an aneurysm, the balloon catheter increases the degree of coil packing in aneurysms with wide necks that were previously considered untreatable by the endovascular approach.
Stents
The development of the Neuroform stent further increased the number of wide-necked aneurysms that would be amenable to embolotherapy. The soft, self-expanding nitinol stent is deployed across the neck of the aneurysm. If the aneurysm is unruptured, the stent is left in place for several weeks to allow the assimilation of the ends of the stent into the arterial walls distal and proximal to the aneurysm neck. This assimilation stabilizes the stent, so that subsequent coil embolization through the interstices of the stent can be performed with greater safety.
Covered stents have yet to be developed for use intracranially, though the Jostent covered coronary graft stent and the Wallgraft covered stent have been used to successfully treat pseudoaneurysms in the cervical segments of the carotid and vertebral arteries (see the image below). Development of a smaller, more distally deliverable covered stent will offer yet another minimally invasive tool to reconstruct arteries and sequester aneurysms from arterial flow.
A, Gunshot wound to the right side of the neck transects the right vertebral artery (RVA) and the right internal maxillary artery (RIMAX), with partial transection and pseudoaneurysm formation in the midcervical right internal carotid artery (RICA). B and C, Transected segments of the RVA and RIMAX are coil embolized. The RICA pseudoaneurysm was successfully treated with a 7 x 40-mm Wallgraft covered stent.
View Media Gallery
Surgical versus coil embolization trials
The results of the International Subarachnoid Aneurysm Trial (ISAT) in 1992 and the International Study of Unruptured Intracranial Aneurysms (ISUIA) in 2003 substantially affected the management of intracranial aneurysms. The randomized, multicenter ISAT trial was designed to compare the safety and efficacy of endovascular coiling with conventional neurosurgical clipping for such aneurysms judged suitable for both treatments. [11] It increased the preference of endovascular therapy as the treatment of primary election in the management of ruptured aneurysms.
In the trial, 2143 patients with ruptured intracranial aneurysms were randomly assigned to neurosurgical clipping (n = 1070) or endovascular treatment with detachable platinum coils (n = 1073). Clinical outcomes were assessed at 2 months and at 1 year. The study showed that 22% of patients survived free of disability at 1 year when they were treated with coil embolization rather than traditional neurosurgical clipping.
In the second of 2 ISUIA studies, unruptured aneurysms were randomized to coil embolization, surgical clipping, or observation. The results showed that among the aneurysms randomized in the treatment arm, an endovascular approach also had a 22% relative risk reduction over conventional surgery, reinforcing the results of the ISAT study.
Flow diversion
Flow diversion is a technique used to treat large or giant wide-necked aneurysms that are not amenable to endovascular coil embolization. Rather than directing treatment toward the lumen of the aneurysm, a stent device is placed in the parent blood vessel across the aneurysm neck. The Pipeline Stent (EV3) is a braided cylindrical mesh, which, when deployed across an aneurysm neck, slows and disorganizes the flow of blood into the aneurysm, which, in turn, promotes thrombosis. Intracranial aneurysms treated with the Pipeline Stent remained occluded in up to 94% of patients at 1-year angiographic follow-up.
Parent vessel sacrifice
Occasionally, aneurysms occur as the result of a blowout of the parent artery. In these cases, reconstruction of the parent artery or endovascular embolization may not be feasible. The remaining alternative of last resort may be occlusion or sacrifice of the parent vessel from which the aneurysm arises.
Success of this technique is dependant on the integrity of the circle of Willis and the ability of the remaining basilar and/or carotid arteries to supply the cerebral arterial distribution of the artery to be sacrificed. This may be readily apparent on diagnostic cerebral angiography if the anterior and/or posterior communicating arteries are identified and widely patent. If these collateral vessels are not readily apparent, sacrifice may still be an option.
To insure adequacy of collateral flow, an intra-arterial balloon test occlusion with concurrent technetium single-photon emission computed tomography (SPECT) imaging may be performed. If the patient fails the test occlusion, then he or she should not be deemed a candidate for permanent parent vessel sacrifice. If the patient does not manifest a focal neurologic deficit over a 30-minute test occlusion, the parent vessel sacrifice will likely be well tolerated by the patient. If the SPECT study shows decreased uptake in that vascular distribution, even if the patient does not manifest a neurologic deficit, the sacrifice will still likely be successful, but would require several days of postembolization hypertensive therapy.
Arterial sacrifice was originally achieved with a trapping procedure using detachable balloons, in which parent vessel occlusion would first be performed distal to the aneurysm to prevent retrograde filling, followed by occlusion proximal to the aneurysm to prohibit antegrade flow to the aneurysm. This same result can now be more easily accomplished with the deployment of 0.035- or 0.038-inch fibered platinum coils such as the Vortex coil (Boston Scientific, Stryker Neurovascular).
STROKE
Dr Abhinav Gupta offers Best treatment for Stroke, from medicines to minimally invasive procedures to cure all patients. Our center is completely equipped with the highly advanced diagnostic technology and accustomed with the extensive therapeutic knowledge possessed by the specialized doctors that helps in treating the patients with the individualized treatments.
Types of strokes covered
Usually, the treatment provided to control and treat the stroke is largely depends upon the type of stroke, you have. Brain and Spine offer variety of treatments for the types of strokes.
- Ischemic stroke
- Hemorrhagic stroke
- Pediatric stroke
- Brain Aneurysm
- Carotid Artery Disease and similar stroke related conditions.
Advanced services from our end
The stroke treatment services at our centre are provided in accordance with the complexity of the stroke, you have. That is why a detailed examination of the patient is done to ascertain the complexity of the stroke and to analyze the safety measures. For this, advanced Interventional, therapeutic and surgical techniques are used for the diagnosis and treatment of the patient.
The patient will be provided with the touch of new approaches of diagnosis and treatment that help him in achieving optimal recovery after the treatment. Our wide range of services cover:
- Neurointensive care unit
- Diagnostic services
- Stroke therapies either through drugs, surgery or Interventional treatment
- Rehabilitation services
- Precautionary advices
- Emergency services
Our center helps the patients with the necessary advices to go with, that makes them attentive towards getting into recurring strokes. It had been seen that stroke survivors are prone to face another stroke. With little attentiveness and a healthy lifestyle, those frequent strokes can be largely avoided. Our center guides the patients and their caregivers with the necessary suggestions, to help them with the feature of stopping those recurring strokes.
Our physiotherapy and rehabilitation department aids in speeding up the recovery of the patient, who have faced a stroke recently. Patients are provided with the after-treatment options to let them gain a fast recovery.
Thrombolytic Therapy for Stroke
The main cause of stroke is blockage of blood supply to the brain due to formation of blood clot. The thrombolytic therapy uses drugs to quickly break the blood clots and dissolve the obstruction to allow blood flow to the brain. This therapy is mainly used for ischemic strokes.
The thrombolytic medications should begin within 3 hours of the first onset of signs and symptoms of stroke. This helps to avoid severe effects of stroke and disability.
Thrombolytic drugs
Depending on the patients need, the type of drug and treatment procedure is decided. Tissue plasminogen activator (tPA) is the common drug used for this therapy. Other than this, drugs commonly used for thrombolytic therapy are:
- Reteplase
- Staphylokinase
- Lanoteplase
- Urokinase
The drug therapy is given only if:
- There is no sign of internal bleeding
- Significant symptoms of stroke have appeared
If the individual suffers from any other medical problem, then usually thrombolytic drug therapy is avoided to reduce risk of damages to other body structures.
Procedure of administration of Thrombolytic therapy:
Thrombolytic therapy uses a long catheter to inject clot-breaking drugs. Initially, these catheters are inserted into the blood vessels and are later guided towards the blood clot. This helps in giving medications directly to the clot. Radiologic imaging is used to examine if the clot is dissolving or not. A small clot can dissolve within few hours but severe blockage may take several days.
Mechanical Thrombectomy is another method which may be opted. This method utilizes a small suction cup, high-speed fluid jet, rotating device or ultrasound device to physically break the clot.
Risk of Thrombolytic Therapy:
A common life-threatening risk of thrombolytic therapy is hemorrhage or bleeding. In almost 25% of the patients undergoing this drug therapy, minor bleeding from nose or gums is seen. Only 1% of the patients may have bleeding in the brain. Other comorbidities in which thrombolysis should be avoided:
- High blood pressure
- Severe bleeding
- Kidney disease
- Recent surgery
The thrombolysis is also not recommended if patient uses blood-thinning medications, or any dietary supplements.
Cerebral Revascularization
.
Stroke therapy summary
National Institute of Neurological Disorders and Stroke (NINDS) recommended target times for patients presenting with an acute neurologic deficit are as follows:
- Door to doctor: 10 minutes
- Door to CT completion: 25 minutes
- Door to CT reading: 45 minutes
- Door to treatment: 60 minutes
- Access to neurological expertise: 15 minutes
- Access to neurosurgical expertise: 2 hours
- Admit to a monitored bed: 3 hours
Acute stroke algorithm (immediate assessment: < 10 min from arrival) is as follows:
- Alert stroke team: Neurologist, radiologist, and CT technician
- Assess airway, breathing, and circulation (ABCs) and vital signs
- Provide oxygen by nasal cannula
- Obtain intravenous access; obtain blood samples (CBC count, electrolytes, coagulation studies)
- Check blood glucose; treat if indicated
- Obtain 12-lead ECG, check for arrhythmias
- Perform general neurological assessment
Immediate neurological assessment (< 25 min from arrival) is as follows:
- Review patient history
- Establish time of onset (< 3 h for fibrinolytic therapy)
- Perform general physical examination
- Perform detailed neurological examination: Determine level of consciousness (Glasgow Coma Scale); determine level of stroke severity (National Institutes of Health [NIH] Stroke Scale or Hunt and Hess Score)
- Order urgent noncontrast CT scan
- Obtain cervical spine radiograph (if comatose or history of trauma)
General therapies for stroke patients are as follows:
- Maintain blood pressure (systolic, 160-180 mm/Hg)
- Titrate fluids and vasoactive agents as needed
- Maintain adequate ventilation (arterial PCO230-35 mm Hg)
- Maintain moderate hypoxia (arterial PO2>100 mm Hg)
- Use lowest positive end-expiratory pressure possible
- Keep arterial pH at 7.3-7.5
- Immobilize (neuromuscular paralysis) as needed
- Sedate as needed
- Anticonvulsants as needed
- Correct blood abnormalities (eg, anemia, electrolytes)
- Monitor and maintain normal serum glucose level
- Give thiamine (100 mg) if malnourished or alcoholic
- Give osmotherapy (mannitol or glycerol) as needed for monitored intracranial pressure elevation or secondary neurologic deterioration
- Avoid hypotonic fluids; avoid excessive fluids
- Keep temperature normal (allow low temperature, treat high temperature)
- Start nutritional support by 48 hours
A critical point is never “normalize” the blood pressure of a patient experiencing an acute neurologic deficit. The target a systolic blood pressure is 160-180 mm Hg.
Fibrinolytic therapy is as follows:
- Systemic intravenous recombinant tissue plasminogen activator (rtPA) with 3 hours (only FDA-approved protocol for cerebral thrombolysis)
- Regional intraarterial tissue plasminogen activator (tPA)/urokinase/abciximab (ReoPro) within 6 hours
- Local intraarterial tPA/urokinase/abciximab within 6 hours
Intravenous tPA therapy includes inclusion criteria and exclusion criteria.
Inclusion criteria for intravenous tPA therapy are as follows:
- Age 18 years or older
- Clinical diagnosis of ischemic stroke causing a measurable neurologic deficit
- Time of symptom onset well established to be less than 180 minutes before treatment would begin
Exclusion criteria for intravenous tPA therapy are as follows:
- Intracranial hemorrhage on noncontrast head CT scan
- Only minor or rapidly improving stroke symptoms
- High suspicion of subarachnoid hemorrhage even if CT scan is normal
- Active internal bleeding (eg, gastrointestinal bleeding or urinary bleeding within last 21 d)
- Known bleeding diathesis, including but not limited to (1) platelet count less than 100,000/µL, (2) received heparin in last 48 hours and elevated partial thromboplastin time, and (3) recent warfarin therapy with prothrombin time greater than 15 seconds
- Less than 3 months since intracranial surgery, head trauma, or previous stroke
- Less than 14 days since major nonneurosurgery or serious trauma
- Less than 7 days since lumbar puncture
- Recent arterial puncture at a noncompressible site
- History of intracranial hemorrhage, AVM, or aneurysm
- Witnessed seizure at onset of symptoms
- Recent acute myocardial infarction
- Systolic blood pressure greater than 185 mm Hg and/or diastolic blood pressure greater than 110 mm Hg; refractory to medications
Intravenous tPA dosage is as follows:
- 9 mg/kg undefined 10% as a bolus over 2 minutes with the remainder infused over 1 hour
Concurrent therapies can include the following:
- Oxygen
- Correct electrolytes
- Maintain vital signs
- Do not treat with anticoagulants (eg, heparin, warfarin, platelet inhibitors [eg, aspirin, clopidogrel])
Intraarterial fibrinolysis therapy includes inclusion criteria and exclusion (relative and absolute) criteria.
Inclusion criteria for fibrinolysis therapy are as follows:
- Diagnosis of ischemic stroke with neurologic deficit undefined within 6 hours of clinical onset
- No age restriction
Relative exclusion criteria for fibrinolysis therapy are as follows:
- Beyond 6 hours of onset (fluctuating)
- Known bleeding diathesis (platelet count < 100,000/µL)
- Presence of an intracranial aneurysm or AVM
Absolute exclusion criteria for fibrinolysis therapy are as follows:
- Identifiable acute infarct or hemorrhage by CT
- Uncontrolled hypertension
- Improving neurologic function
Medical care for patients with stroke had historically focused on limiting the extent of the stroke with volume expansion and anticoagulation followed by rehabilitation. Until recently, no therapy directed at stroke reversal was available to this large segment of the population. Given the tremendous strides made in the areas of cardiac and limb salvage over the past decade, a number of modalities are now directed at reestablishing cerebral blood flow. If accomplished quickly enough, neurologic function may be restored.
Intra-arterial cerebral revascularization incorporates several new technologies and new applications of techniques that have been well established in the field of peripheral revascularization. The focus on acute stroke reversal offers a challenge to interventional Neuroradiology, whereby thrombolytic therapy delivered selectively only to the occluded vessel provides recanalization in a fraction of the time, with a significant reduction in total dosage and with fewer complications than are associated with intravenous thrombolytic therapy.
The most important factor affecting the successful outcome of any reperfusion therapy is the early diagnosis of a stroke in progress and the patient’s arrival to a hospital that can offer these therapies as quickly as possible. Public education must be a priority to alert not only high-risk individuals but also their families to the availability of acute care with the potential to reverse a stroke. For this reason, many national stroke organizations have redefined stroke as a “brain attack.” The phrase heart attack now evokes the idea of angioplasty, coronary bypass, and newer medical therapies. People have come to expect that a heart attack can be reversed. The hope is that using the phrase “brain attack” will evoke similar expectations that stroke is a treatable disorder and that thrombolytic therapies, as well as mechanical thrombectomy, angioplasty, and stenting, may reverse an acute stroke in progress.
Commonly used agents
The most thrombolytic agents are those classified as plasminogen activators and historically included streptokinase, urokinase, and rt-PA (see the image below). Streptokinase is no longer used or available because of its tendency to cause hypersensitivity reactions. Although effective, and associated with a lower hemorrhagic conversion rate than rt-PA, urokinase is also no longer available. Prourokinase is a genetically engineered variant of urokinase. The Prolyse in Acute Cerebral Thromboembolism (PROACT) trial showed that prourokinase was effective in treating cerebral intraarterial thrombolysis. For reasons that still confound the author, Prourokinase was never made available for use in the treatment of stroke outside of the PROACT trials. [12, 13]
A 47-year-old woman had a sudden onset of left hemiplegia while in the ICU. She was excluded from the intravenous tissue-type plasminogen activator (tPA) protocol because she recently underwent heart-lung transplantation. A, Right internal carotid angiogram demonstrates occlusion of the right middle cerebral artery. B and C, Flow is reestablished at 28 minutes after selective infusion of urokinase into the right middle cerebral artery. The patient recovered neurologic function while she was still on the angiography table.
View Media Gallery
Currently, the only fibrinolytic agent available for intraarterial thrombolysis is rt-PA. Intraarterial tPA therapy is often augmented with the use of abciximab. Abciximab is a platelet aggregation inhibitor, which, when applied to an acute thrombus, appears to also have platelet antiaggregate properties. In the author’s program, the concurrent use of up to 10 mg of abciximab directly into the clot within an occluded vessel or proximal to the clot in a recanalizing vessel has contributed to a significant reduction in the amount of intraarterial rt-PA infused, which, in turn, has led to a reduction in the rates of hemorrhagic conversions.
Thrombolytic protocols
A number of protocols are in effect for the intravenous administration of thrombolytic agents, most notably rt-PA. These methods establish a systemic lytic state with relatively large doses of thrombolytic agents. Risks include lysis of thrombi anywhere in the body, including the musculature, lungs, and abdominal viscera, as well as in peptic ulcers and recent wounds. Evidence suggests an increased incidence of hemorrhagic conversion of strokes older than 6 hours when treated with IV rt-PA. The FDA subsequently approved the use of r-tPA in strokes of less than 3 hours’ duration.
In May 2009, the American Heart Association/American Stroke Association (AHA/ASA) guidelines for the administration of rt-PA following acute stroke were revised to expand the window of treatment from 3 hours to 4.5 hours to provide more patients with an opportunity to receive benefit from this effective therapy. [14, 15, 16,17]
Eligibility criteria for treatment in the 3-4.5 hours after acute stroke are similar to those for treatment at earlier periods, with any 1 of the following additional exclusion criteria:
- Patients older than 80 years
- All patients taking oral anticoagulants are excluded regardless of the international normalized ratio (INR)
- Patients with baseline NIH stroke scale score greater than 25
- Patients with a history of stroke and diabetes
“Drip & ship”
Patients admitted and imaged at hospitals unequipped to provide dedicated stroke care may be given a half a dose of intravenous tPA and transferred to a stroke center. On arrival, depending on the patient’s response to the initial half dose of tPA, the patient may receive supportive therapy, volume expansion, anticoagulant with or without antiplatelet therapy, the second half dose of intravenous tPA, or endovascular therapy.
Delivery of thrombolytic agents
The intraarterial delivery of thrombolytic agents allows for the administration of smaller volumes of more concentrated thrombolytic agent over a shorter period beyond the 3-4.5 hour limitation of the intravenous tPA protocol. Concurrent anticoagulant therapy and platelet inhibition appear to augment the effects of locally infused lytic agents. While the use of anticoagulants and platelet inhibitors is not approved with the intravenous rt-PA protocol, their use in intraarterial therapy appears to augment the effectiveness of intraarterial thrombolytic therapy, recanalizing vessels more rapidly and possibly promoting a more complete neurologic recovery with fewer complications.
The arterial route offers the distinct advantage of infusing the drug directly into the clot, accelerating the restoration of flow. A systemic lytic state is not produced; therefore, the risks of hemorrhage at other sites, though not eliminated, are markedly reduced. Extensive research is under way to develop agents that are clot specific and that can lyse thrombi even more rapidly with fewer adverse effects.
Selective intraarterial dissolution of thrombus has also been achieved with the newer antiplatelet agents. Abciximab, as previously discussed, is an antiplatelet agent that has thrombolytic properties similar to those of the plasminogen activators. Lower intraarterial doses of plasminogen activator may be given concurrently, which may lead to a lower incidence of hemorrhagic complications. This technique has become the preferred intraarterial chemothrombolytic management of thromboembolic stroke in the author’s institution.
In the author’s experience, the apparent rate at which a clot lyses with a plasminogen activator appears to decline as flow across the thrombosed vessel improves. This has led to speculation that the in vivo activation of plasminogen to plasmin may not be as instantaneous as believed. The progressive reduction in clot lysis as flow improved suggests that at a portion of the plasminogen activation does not occur until after it has passed the clot, making it less effective as a local thrombolytic procedure.
In 2005, this author completed a study evaluating a technique for accelerating thrombolysis with even smaller volumes of the lytic drug. The study involved the in vitro preactivation of plasminogen in autologous blood to active plasmin. The subsequent infusion of the admixture containing preactivated plasmin appears to enhance thrombolysis in vessels that have begun to recanalize, suggesting improved surface contact of plasmin on the clot. The technique is anticipated to accelerate arterial recanalization and neurologic recovery with a lowered risk of hemorrhagic complications in the acute setting.
Nonthrombolytic techniques
Nonthrombolytic techniques include low-pressure angioplasty of the thrombus and mechanical thrombectomy. A variety of compliant and noncompliant balloon catheters are available in sizes of 2-10 mm to allow access to both the cervical and the primary branches of the intracranial arterial anatomy. Angioplasty rapidly remodels the thrombus to reestablish flow, but it does not entail extraction or dissolution of the thrombus. Risks include distal embolization by fragmented thrombus and occlusion of small perforator branches of the circle of Willis.
Mechanical thrombectomy devices include the AngioJet and Neurojet devices. These tend to be most applicable in the large vessels of the neck. These devices, however, are cumbersome and poorly navigable and have little application in the current management of stroke. The Merci Retriever is capable of significantly greater distal access to the intracranial arterial and venous anatomy. Designed to extract a clot in a state of flow arrest, the Merci device has contributed to a significant reduction in time to recanalization while reducing and often eliminating the need for chemothrombolysis and its associated risk of hemorrhagic complications. The Merci device also inspired development of newer, more effective, and more navigable endovascular thrombectomy devices.
See the image below.
Penumbra System mechanical thrombectomy device. Used with permission from Penumbra, Inc.
View Media Gallery
The Penumbra (Penumbra, Inc) uses a bulbous separator mounted on a guidewire, which is passed through a microcatheter and repeatedly advanced and withdrawn across an occluded segment of vessel. The process is designed to mechanically disrupt the thrombus and aspirate the liberated fragments through the delivery catheter, which is maintained under continuous negative pressure.
More recently, stent retriever devices have been introduced. [18] The Solitaire stent retriever (EV3) is designed to grab and extract a thrombus with a technique similar to the Merci device. Delivery guidewires with open-ended Solitaire stents of various sizes permanently affixed facilitated more distal access and an improved rate of successful clot extraction. The Trevo Stentriever (Concentric Medical, Stryker Neurovascular) is an open-ended stent retriever with the advantage of being available in a single stent diameter designed to fit a wider range of vessel diameters, a feature that reduces the amount of inventory needed. Both the Solitaire and Trevo devices are intended to be used in a state of flow arrest, with clot extraction facilitated by aspiration of a balloon-occlusive guide catheter during withdrawal.
Angioplasty and stent placement
An integral part of cerebral revascularization is the treatment of the source of an embolus, most commonly cardiogenic or carotid-vertebral atheroocclusive disease. Technological advances have made angioplasty and stenting of proximal arterial stenoses in carotid and vertebral vessels as fast and as easy a process possible. Dilation of the thromboembolic foci increases cerebral perfusion pressure and cerebral blood volume and reduces the risk of reembolization and reocclusion.
A number of trials have shown the effectiveness of the Xact Carotid Stent System, the RX Acculink Carotid Stent System, and the RX Accunet Embolic Protection System in repairing a stenosis with a distal protection device capable of capturing liberated atheromatous debris.
The Acculink for Revascularization of Carotids in High Risk Patients (ARCHER) trial was designed to evaluate stent reconstruction as a minimally invasive alternative to treat carotid artery stenosis in patients in whom conventional carotid endarterectomy posed a high risk for perioperative complications. Eligible patients who were symptomatic or asymptomatic were considered to be at high risk if they met 2 or more of the following criteria [19] :
- Two or more coronary vessels with 70% stenosis
- Myocardial infarction within 30 days with a concurrent requirement for coronary artery bypass grafting or valve surgery within 30 days
- Unstable angina
- Occlusion of the contralateral internal carotid artery
Inclusion criteria defining high-risk patients also included one or more of the following [19, 20, 21, 22, 23,24] :
- Ejection fraction of less than 30%
- Forced expiratory volume of less than 30%
- Dialysis-dependent renal failure
- Uncontrolled diabetes
- Restenosis after carotid endarterectomy
- Previous radical neck surgery and/or radiation therapy
- Surgically inaccessible lesions
- Spinal immobility
- Tracheostomy stoma
- Paralysis of the contralateral laryngeal nerve
Patients are given aspirin 325 mg twice a day and clopidogrel 75 mg twice a day for 48 hours prior to the stent procedure. During the procedure, an activated clotting time (ACT) of 250 seconds was maintained with heparin. After the procedure, patients were prescribed a daily regimen of aspirin 325 mg for a minimum of 1 year and clopidogrel 75 mg for a minimum of 2-4 weeks. [19]
The 30-day total major adverse event rate, defined as all-causes of stroke, death, and myocardial infarction, was 7.8%. The success rate with the Acculink device, defined as successful deployment of the stent and less than 50% residual stenosis, was 97.8%. The success rate for delivery, placement, and retrieval of the Accunet device was 92.7%. About 57% of retrieved filters contained debris. [19]
The ARCHER trial is one of the first trials conducted to study stenting of the carotid artery in patients who are high-risk candidates for carotid endarterectomy. The 30-day major adverse event rate of 7.8% compares favorably with outcomes in similar high-risk carotid endarterectomy in which rates of stroke, death, and myocardial infarction exceeded 10%. These results demonstrated that carotid stenting with filter protection can be safely performed in high-risk surgical patients and contributed to subsequent FDA approval of the Acculink and Xact stent systems for use in carotid stenosis. [19]
Vertebroplasty and Kyphoplasty
Vertebroplasty and Kyphoplasty are FDA-approved techniques for vertebral reconstruction that involve the injection of bone cement into abnormal vertebral bodies of the spine. The procedures are most commonly performed to treat painful vertebral compression fractures that have not responded to conventional therapies such as bed rest, bracing, or analgesia. The fractures are typically caused by osteoporosis; however, occasionally fractures due to trauma and tumors, such as metastases, multiple myelomas, and hemangiomas, can be treated to reduce the associated pain. Neither vertebroplasty nor kyphoplasty are intended for the treatment of pain due to disk disease. [25, 26, 27, 28, 29, 30, 31]
Inclusion and exclusion criteria are the same for vertebroplasty and kyphoplasty. Inclusion criteria include pain localized to fracture or tumor, pain refractory to medical management, and fracture less than 12 months old. Exclusion criteria include fracture extending to the posterior vertebral cortex, retropulsed fragment, cord compression, symptoms limited to radicular pain, infection (fever, sepsis, abscess, diskitis-osteomyelitis), pain that responds to minimal analgesia, coagulopathy, and penetrating trauma.
Vertebroplasty
Vertebroplasty consists of the transpedicular or peripedicular placement of an 11-gauge (lumbar) or 13-gauge (thoracic) needle into the anterior third of the affected vertebral body under radiographic guidance (fluoroscopy or CT). Once positioned, bone cement, methylmethacrylate, is injected through the needle into the vertebral body (see the image below). Methylmethacrylate is a medical-grade polymer that has been used for more than 30 years in artificial joints and cranioplasty. The cement is mixed with a powder containing barium to enhance the radiographic visibility. Radiopacity may be further enhanced with the addition of tantalum or tungsten powder.
A and D, Osteoporotic anterior wedge compression fractures. B, Placement of a needle into the collapsed vertebral body. E and R, Result after the injection of methylmethacrylate. This therapy is principally indicated for the management of pain. C, The primary goal is to fuse the fracture fragments to prevent their continued motion. F, Vertebroplasty occasionally elevates the superior endplate of an acute fracture, reducing kyphotic deformity. A, B, and C modified from Netter.
View Media Gallery
When injected, the material initially has the consistency of toothpaste. After approximately 10 minutes, the cement solidifies, becoming harder than the native bone. Following the procedure, the patient is kept supine for 3 hours and discharged to home. The procedure is not painful and requires only local and deep anesthesia with mild sedation and analgesia.
In most cases, the pain is reduced or eliminated immediately after the procedure. Patients must still exercise caution in subsequent activities, because other osteoporotic vertebral bodies may be prone to fracture. Medical management of the underlying medical disorder that weakened the vertebral bodies should be initiated. The risks of the procedure are low but potentially include infection, worsening of pain, and neurologic sequelae such as weakness or pain.
Kyphoplasty
Kyphoplasty, like vertebroplasty, is intended to treat the pain of vertebral compression fractures with the hypothetical added advantage of restoration of vertebral height and reduction the exaggerated kyphotic curvature of the spine caused by an anterior wedge compression fracture. This effect is accomplished with the placement of 1 or 2 high-pressure balloons into the fractured vertebral bodies. When inflated, the balloons create a cavity within the trabeculae, theoretically resulting in a separation of the fracture fragments. A thicker preparation of methylmethacrylate than used in vertebroplasty is then injected into the bone with the same technique as that described above. This technique is limited to acute compression fractures, and it is not intended for the treatment of neoplastic lesions of the vertebrae.
Percutaneous Diskectomy
Back pain related to a herniated intervertebral disk is one of the most common causes of chronic disability. Although many cases of acute low back pain resolve with conservative therapy, surgical decompression is often considered when the pain is unimproved after physical therapy and when the characteristics of the pain clearly suggest a neuropathic origin.
Open surgery was historically used to treat radicular pain with diskectomy (ie, removing part of the abnormal intervertebral disk) or with decompressive laminectomy (ie, resecting portions of the lamina to relieve the pressure on the spinal canal and nerve roots). Initial surgical success rates have been in excess of 90%; however, conventional surgical techniques have been associated with an approximate 17% incidence of failed back syndrome, in which symptoms recur as a consequence of scar formation in the operative bed, compromising the adjacent nerves. Decompressive surgical techniques have advanced to the point where procedures using laser or radiofrequency energy are performed through small incisions or with endoscopy. These newer, less invasive surgical techniques have been associated with a lower incidence of failed back syndrome than open surgical decompressive therapies.
Percutaneous disk decompression has been used to treat herniated nuclei for over 40 years in more than 500,000 patients. A variety of techniques have been used, including chemical, mechanical, and thermal methods, including radiofrequency and laser ablation. Early procedures conclusively showed that percutaneous disk decompression effectively relieves pain for appropriate patients.
Intradiskal electrothermal annuloplasty (IDET) is another older minimally invasive approach to treat low back pain. In this treatment, a heated element is used to treat pain thought to arise from sensory nerves in the surrounding annulus. This procedure has had limited clinical success.
The Nucleotome system, the Dekompressor percutaneous diskectomy probe, and the Disc Nucleoplasty device are examples of FDA-approved percutaneous diskectomy devices. The last 2 are the ones that are most commonly used. None of the techniques using these devices, surgical or percutaneous, are targeted at the extruding disk fragment; rather, they are designed to reduce the volume of the residual nonherniated nucleus pulposus remaining within the annulus, in an attempt to reduce pressure on the herniated fragment during load bearing.
Percutaneous disk decompression ha s been used to treat symptomatic patients with contained herniated disks. The ideal patient meets the following common criteria: radicular symptoms (eg, leg pain greater than back pain), CT or MRI evidence of contained posterolateral disk protrusion and 1 failed selective nerve-root block (included to ensure that the patient’s condition is given the opportunity to respond to conservative care), failed conservative therapy for 3 months, and diskographic findings positive for concordant pain .
Exclusion criteria include disk height of less than 50%, evidence of severe disk degeneration, spinal stenosis, traumatic spinal fracture, infection, tumor, pregnancy, and severe coexisting medical disease. The procedure is not indicated for the treatment of pain originating from structures other than herniated disks. Patients with a free disk fragment or with severe and rapidly progressing neurologic deficits are excluded.
Potential complications include infection, bleeding, nerve damage, worsening of pain, paralysis, idiosyncratic reaction, anaphylaxis, and death.
The procedure should be performed with the patient under local anesthesia or conscious sedation to allow the patient to participate in monitoring for signs of segmental nerve root irritation. After the device is inserted under fluoroscopic guidance into the disk space, disk decompression is performed in only a few minutes. The entire procedure lasts about 30 minutes per level, and the patient can be discharged shortly afterward. Patients typically have little pain after the procedure, and any pain is usually managed with analgesics. Patients are advised to avoid lifting and strenuously exercising, and they may go back to sedentary work after one week. Patients with physically demanding occupations may need to wait longer than this to recommence their daily activities. Additional physical therapy may prove beneficial in the recovery period.
Percutaneous diskectomy may decrease procedural time, need for anesthesia, and recovery time; may lower the complication and morbidity rates; and may substantially reduce postoperative spinal instability. Percutaneous diskectomy has demonstrated the potential to produce outcomes equivalent to or better than those of conventional decompressive surgery. The procedure is permanent, simple, quick, and relatively atraumatic, with less perineural scarring and postoperative fibrosis and shorter recovery times. Clinical results are promising, and patients can generally expect rapid and sustained pain reduction.
Dekompressor
The Dekompressor percutaneous diskectomy probe (Stryker) uses a self-contained motorized drill to remove nucleus pulposus from the annular compartment through a small channel under fluoroscopic guidance. Superficial, deep, peridiskal and intradiskal anesthesia is provided with lidocaine. Diskography is first performed to define the margins of the nuclear compartment. The cannula is then advanced into the disk space by using a posterolateral approach into the thoracic or lumbar intervertebral disk space. As the device is activated, the drill bit disrupts nuclear tissue and mechanically draws the material into a collection chamber at the base of the motor assembly. Patients rarely have any discomfort during the procedure. The probe is capable of aspirating disk material from the intervertebral disk spaces of the lumbar, thoracic, and cervical spine. [32, 33, 34]
Nucleoplasty and Coblation
DISC Nucleoplasty (ArthroCare) uses a unique plasma technology called Coblation to remove tissue from the center of the nucleus pulposus. During the procedure, a probe is introduced through a needle and placed into the center of the disk, where a series of channels are created to remove tissue from the nucleus. This Coblation plasma technology has been used for many years in arthroscopic surgical procedures and in otolaryngologic procedures. Coblation decompresses the disk while preserving adjacent healthy tissue by using plasma energy rather than heat energy to remove tissue. [35, 36]
The disk is accessed through a 17-gauge (cervical or thoracic) or 19-gauge (lumbar) cannula with an obturator stylet by using an anterolateral approach in the cervical spine or a posterolateral approach in the thoracolumbar spine. While the patient is monitored, the probe is advanced into the disk. As the probe is advanced, the Coblation plasma mode is activated, and tissue along the path of the device is removed by means of molecular dissociation.
Tissue is turned into gas, which exits the disk through the introducer cannula. After reaching a predetermined depth, the probe is slowly withdrawn to the starting position. Sufficient thermal energy is generated to denature nerve fibers adjacent to the channel in the nucleus pulposus. After the first channel is created, the probe is rotated clockwise and readvanced to create another channel. Approximately 6 channels are made, depending on the amount of tissue reduction desired.
Since its first application in July 2000, outcome studies showed high success rates worldwide. Average pain reduction is a clinically significant 55-60%. Patient satisfaction is high, about 90%, largely because of the relative ease of the procedure, because of the lack of painful rehabilitation period, and because the procedure does not preclude subsequent procedures (eg, open surgery). Early studies showed that pain relief is sustained for as long as 2 years after surgery.
Nucleotome
The Nucleotome system (Clarus Medical) involves a percutaneous approach to rapidly remove nucleus pulposus from a lumbar intervertebral disk. The probe of the system has a rounded tip that reduces the risk of penetrating the anterior annulus. A vacuum draws nucleus material into a cutting port while the reciprocating, enclosed guillotine resects and aspirates portions of the nucleus. The action does not damage the annulus or endplates. Continuous irrigation removes aspirated material from the probe and allows the physician to collect and examine the extracted tissue.
Performed under local anesthesia, this procedure was traditionally surgical; however, its potential as a fluoroscopically guided procedure warrants consideration.
More than 125,000 procedures have been performed worldwide without a reported treatment-associated death. Success rates have been greater than 75%. Complication rates for this technique are consistently reported to be less than 1%, a considerable reduction from the normal 3-4% reported for open spinal surgery
